Breast Health & Well-Woman Care Guide USA 2026
Breast Health and Well-Woman Care: The Ultimate 2026 Guide

Introduction
Breast health is a cornerstone of overall well-woman care. Understanding and maintaining breast health through regular self-exams, clinical screenings, and awareness of warning signs can help detect problems early and support lifelong wellness. In 2026, integrating breast health practices into your daily routine is easier than ever with clear guidelines, lifestyle strategies, and modern preventive care.
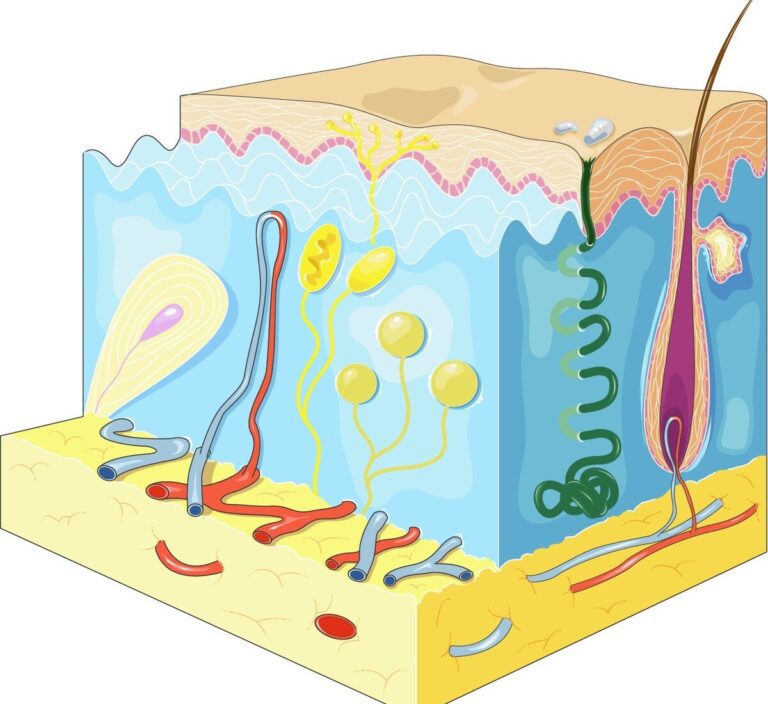
Understanding Breast Anatomy and Function
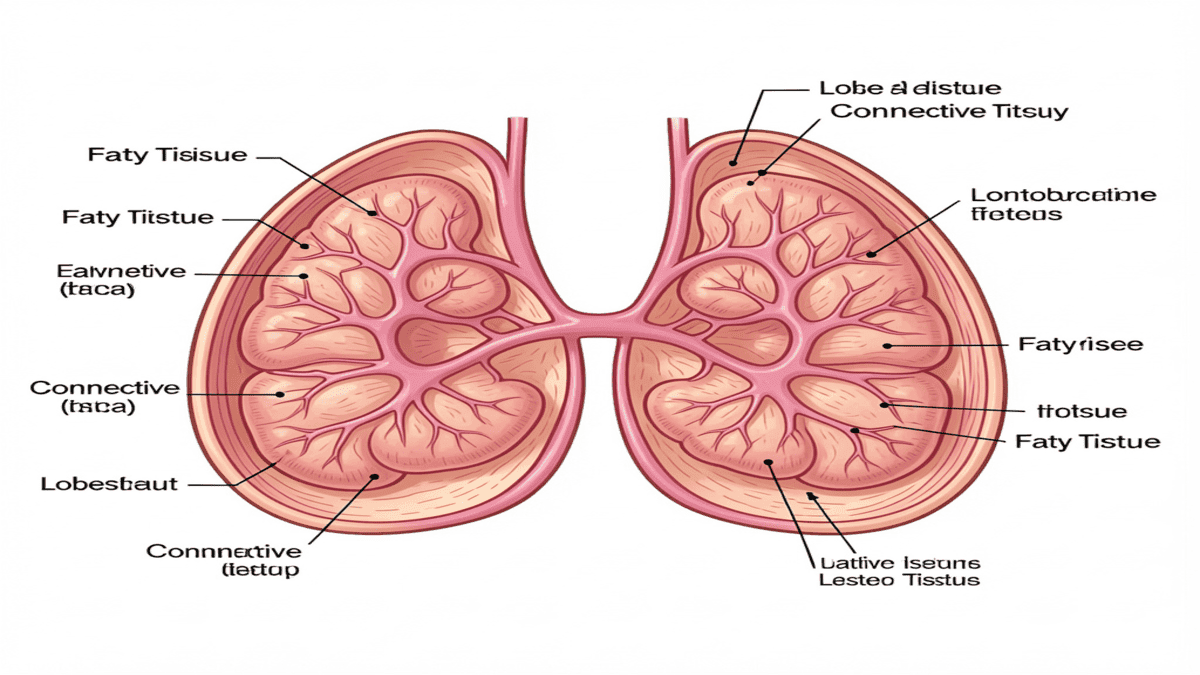
Your breasts are more than a physical feature—they are complex organs essential for breast health, reproduction, and hormonal balance. Understanding their structure and function helps women recognize normal changes, maintain healthy breasts, and detect potential problems early, supporting overall well-woman wellness.
1. Basic Structure of the Breast
- Lobes and Lobules: Each breast contains 15–20 lobes, divided into smaller lobules that produce milk.
- Ducts: Milk travels from the lobules through ducts to the nipple.
- Fatty Tissue: Surrounds lobes and ducts, giving breasts their shape and size.
- Connective Tissue: Supports breast structure and maintains shape.
Tip: Breast density varies by age, genetics, and hormonal status, which can affect how lumps are felt during exams—knowing your normal tissue is key for breast health awareness.
2. Hormonal Influence on Breasts
Breast tissue responds strongly to hormones throughout life:
- Estrogen and Progesterone: Cause swelling and tenderness before menstrual periods.
- Prolactin: Stimulates milk production during pregnancy and breastfeeding.
- Menopause: Reduced estrogen can decrease breast density and firmness.
Tip: Understanding these changes helps distinguish normal variations from warning signs, supporting healthy breasts over a lifetime.
3. Common Changes in Breasts
Women may notice changes due to normal physiological processes:
- Cyclical tenderness or lumpiness before periods
- Enlargement during pregnancy or breastfeeding
- Slight asymmetry (one breast larger than the other)
Red Flag: Sudden lumps, persistent pain, nipple discharge, or skin changes should always be evaluated by a doctor to protect your breast health.
4. Breast Types and Shapes
- Breasts vary in size, shape, and tissue composition.
- Common types: Rounded, teardrop, asymmetrical, or pendulous.
- Tissue composition (fatty vs. dense) affects self-exam technique and mammogram readings.
Tip: Knowing your normal breast shape and texture makes it easier to detect unusual changes, contributing to better breast health awareness.
5. Why Understanding Anatomy Matters
- Improves effectiveness of self-exams
- Helps interpret changes during screenings
- Supports informed discussions with healthcare providers
- Encourages proactive well-woman care and breast health
Breast Self-Exams: Step-by-Step
Performing regular breast self-exams is one of the most effective ways to support breast health and detect changes early. Here’s a detailed guide to make it simple and effective, helping you maintain healthy breasts throughout your life.
1. Why Self-Exams Matter
- Helps you become familiar with your normal breast shape, size, and texture.
- Early detection of unusual lumps or changes can improve treatment outcomes and protect breast health.
- Complements professional screenings like mammograms and ultrasounds.
Tip: Perform a self-exam once a month, ideally a few days after your period when breasts are less swollen, to maintain breast wellness.
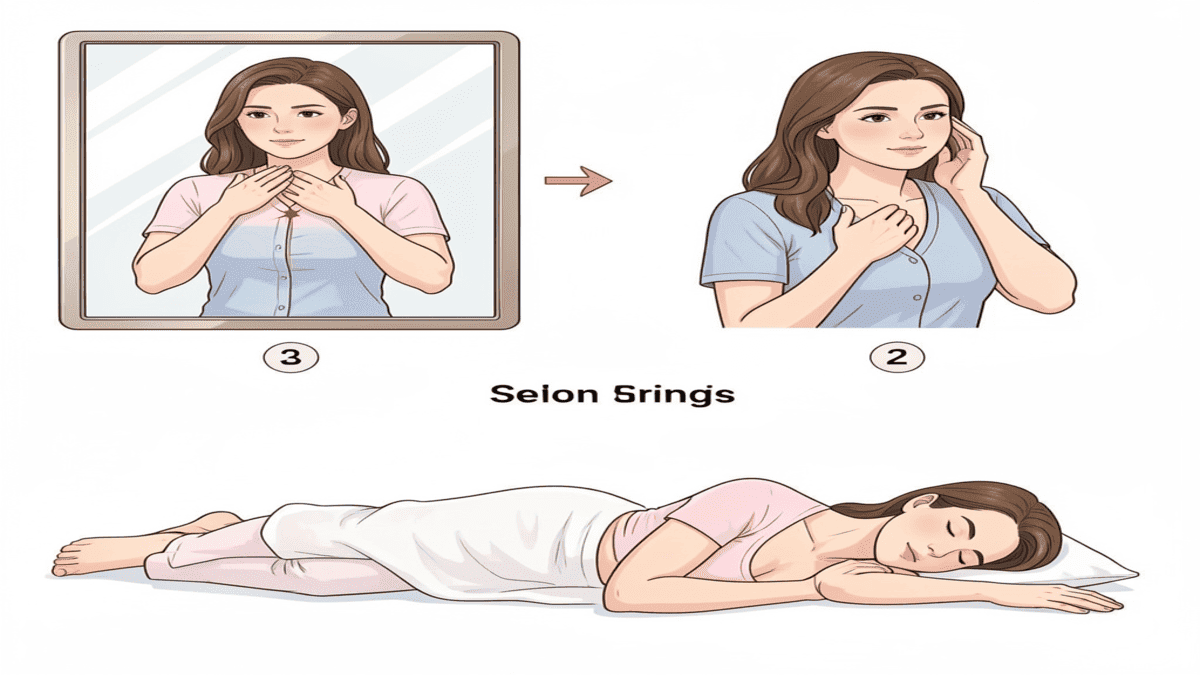
2. Visual Inspection

- Place your arms on your hips and your shoulders erect as you face a mirror.
- Look for:
- Swelling or asymmetry
- Skin dimpling or puckering
- Changes in nipple shape or color
- Raise your arms and check for the same changes from different angles.
Tip: Proper lighting and posture make a big difference—this helps you keep track of breast health changes effectively.
3. Palpation While Lying Down
- Lie flat on your back with a pillow under your shoulder on the side being examined.
- Use pads of your fingers, not fingertips, and apply light, medium, and firm pressure.
- Move in small circular motions covering the entire breast, including:
- Outer edges
- Under the armpit (axillary region)
- Around the nipple
- Repeat on the other breast.
Tip: Using a pattern (circular, wedge, or vertical lines) ensures no area is missed, keeping your breast health monitoring thorough and consistent.
4. Palpation While Standing or in the Shower
- Wet, soapy skin makes it easier to feel lumps or thickened tissue.
- Use the same technique as lying down, covering the entire breast and armpit.
Tip: Many women find the shower method easiest for remembering monthly self-exams, which is key for ongoing breast health.
5. What to Watch For
- Lumps or thickened areas not present before
- Persistent pain or tenderness
- Nipple discharge (especially bloody or clear fluid)
- Changes in skin texture, dimpling, or redness
Red Flag: Any of these signs should prompt a visit to a healthcare provider immediately to protect your breast health.
6. Record Your Findings
- Keep a breast health journal or app to track changes monthly.
- Note: date, location, size, texture, and any associated symptoms.
- Over time, this helps you and your doctor detect trends or abnormalities early.
Tip: Photos or diagrams can be helpful for reference if changes occur, supporting breast wellness tracking.
7. Combining Self-Exams with Professional Care
- Self-exams do not replace mammograms or doctor visits.
- To find the ideal screening schedule, talk to your healthcare physician about your risk factors.
- High-risk women may need earlier or additional imaging.
Tip: Integrating self-exams with professional care ensures comprehensive breast health monitoring.
Screening and Diagnostic Tests for Breast Health
Regular screenings are essential for breast health and early detection of breast issues, including cancer. Understanding the types of tests, their purpose, and when to get them helps women make informed health decisions and maintain healthy breasts throughout life.
@@@@@@@@@1/1
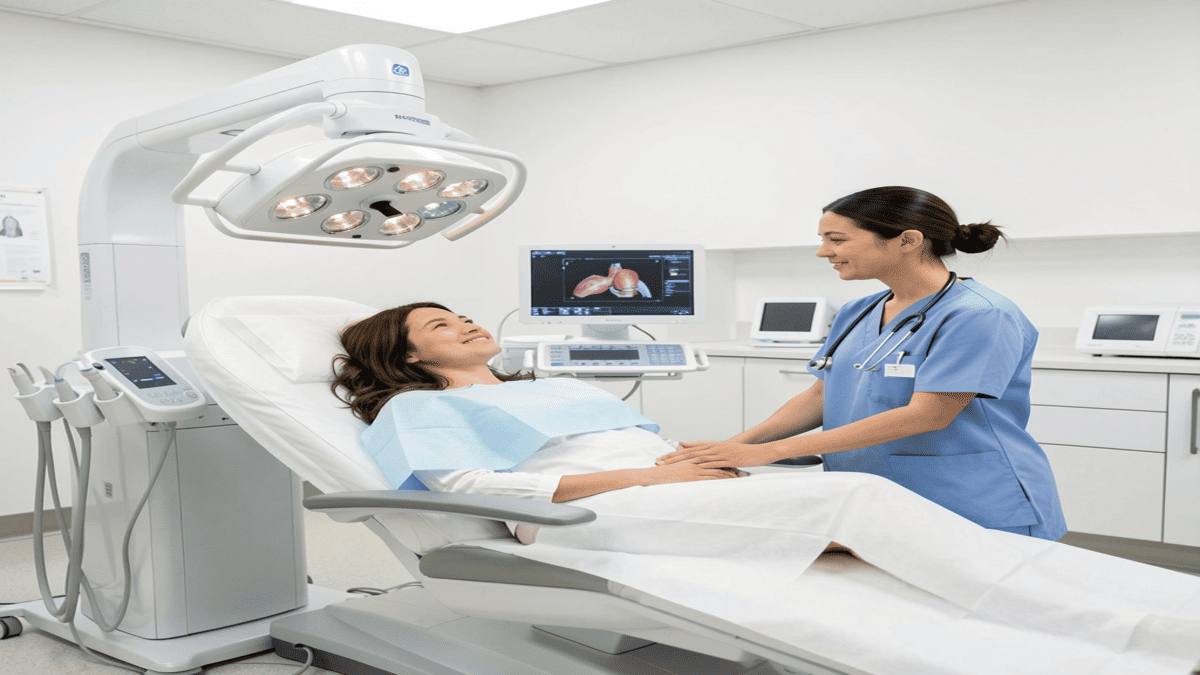
1. Mammograms: The Standard Screening Tool
- What it is: A low-dose X-ray of the breast used to detect lumps or abnormalities.
- Who needs it: Women aged 40+ at average risk; earlier if family history or high-risk factors exist.
- Frequency:
- Every 1–2 years for average-risk women
- Yearly for women at higher risk
- What to expect: Slight compression of the breast for clear images; typically quick and safe.
Tip: Schedule your mammogram at the same time each year, ideally one week after your period when breasts are less tender. Regular mammograms are a cornerstone of breast health monitoring.
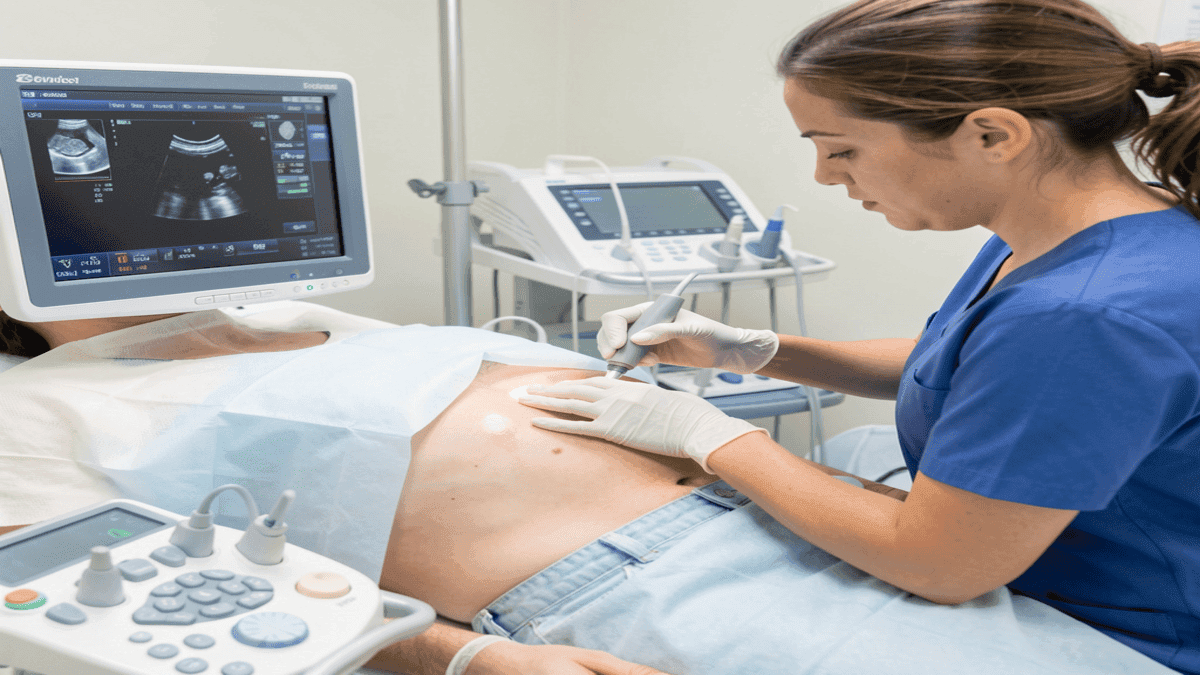
2. Ultrasound: Supplemental Imaging
- Purpose: Helps distinguish between fluid-filled cysts and solid masses.
- Often used if mammogram results are unclear or for dense breast tissue.
- Procedure: Non-invasive, painless, uses sound waves to create images.
Tip: Ideal for younger women or those with dense breasts, as mammograms can sometimes miss abnormalities. Ultrasound is an excellent tool to support breast health in women with dense tissue.
3. Breast MRI: Advanced Screening
- Purpose: Highly sensitive imaging, often used for women at high risk (e.g., BRCA1/BRCA2 gene mutations).
- Can detect small or early-stage cancers not seen on mammograms or ultrasound.
- Procedure: Involves lying in a scanner; contrast dye may be used.
Tip: Usually recommended in addition to mammograms for high-risk patients, not as a replacement. Advanced imaging is an important part of maintaining healthy breasts for high-risk women.
4. Clinical Breast Exams (CBE)
- Performed by a healthcare professional during routine check-ups.
- Helps detect lumps or changes that may not be noticeable on self-exams.
- Frequency: Often every 1–3 years for women aged 20–39, yearly for women 40+.
Tip: Pair self-exams with CBEs to increase the chance of early detection and overall breast health monitoring.
5. Genetic Testing and Risk Assessment
- Women with a family history of breast or ovarian cancer may consider testing for BRCA1, BRCA2, and other genes.
- Helps guide personalized screening schedules and preventive strategies.
- Genetic counseling is recommended before and after testing.
Tip: Even without a positive gene, maintaining a healthy lifestyle and following breast health guidelines is essential.
6. Choosing the Right Screening Plan
- Discuss your personal and family history, age, and risk factors with your doctor.
- High-risk women may need earlier, more frequent, or additional imaging.
- Low-risk women can follow standard guidelines for mammograms and exams.
Tip: Keep a record of all imaging tests to track changes over time and support ongoing breast health.
7. Key Takeaways
- Combine self-exams, clinical exams, and imaging for the most effective early detection of breast changes.
- Early detection significantly improves outcomes for breast cancer and other conditions.
- Following USA 2026 guidelines ensures up-to-date practices for breast health monitoring.
Common Breast Conditions and Breast Health Awareness
While most breast changes are benign, it’s important to recognize what’s normal and what may need medical attention. Understanding common conditions supports breast health, helps women maintain healthy breasts, and allows for timely medical evaluation when needed.
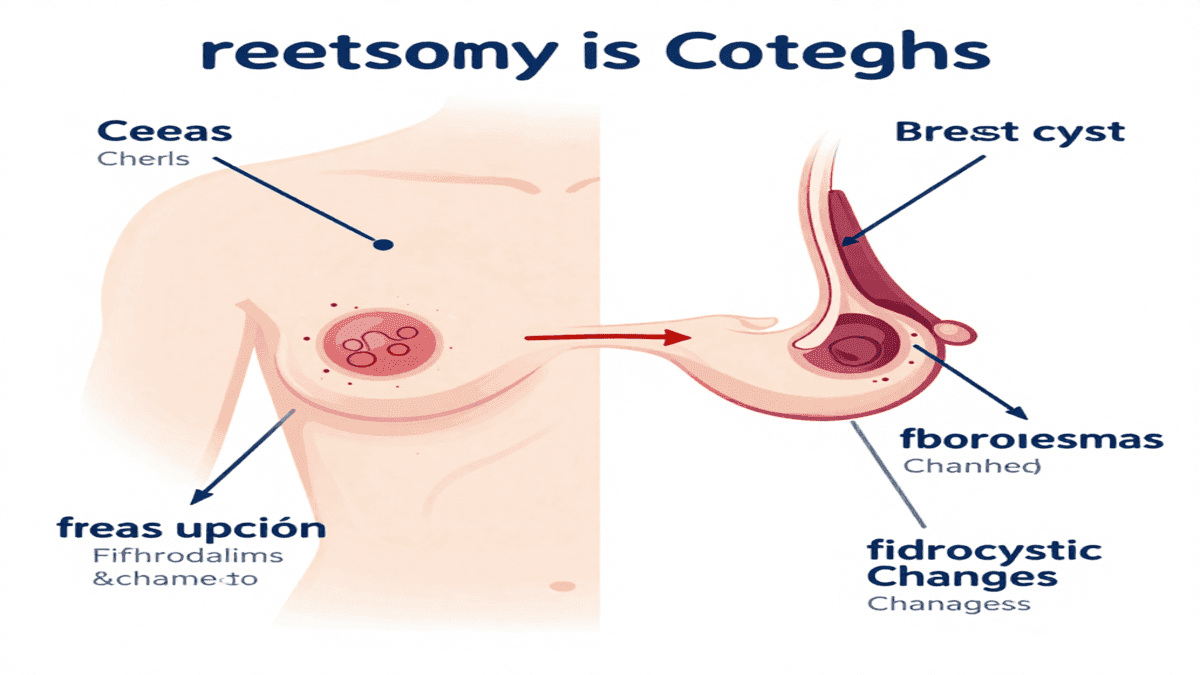
1. Breast Cysts
- What they are: Fluid-filled sacs within the breast tissue.
- Symptoms: Smooth, round lumps that may be tender, especially before periods.
- Diagnosis: Usually detected via ultrasound; mammograms may also show cysts.
- Management: Often resolve on their own; your doctor may aspirate fluid if painful.
Tip: Track cyclical tenderness and lump size to distinguish normal cysts from concerning changes and support ongoing breast health monitoring.
2. Fibroadenomas
- What they are: Solid, non-cancerous lumps most common in women aged 15–35.
- Symptoms: Firm, smooth, and movable lumps; usually painless.
- Diagnosis: Ultrasound, mammogram, or biopsy if uncertain.
- Management: Often monitored; removal considered if growing or causing discomfort.
Tip: Fibroadenomas are benign but still require monitoring for any changes in size or texture to maintain healthy breasts.
3. Fibrocystic Breast Changes
- What it is: Lumpy or rope-like breast tissue due to hormonal fluctuations.
- Symptoms: Swelling, tenderness, and lumpiness, often worsening before periods.
- Diagnosis: Clinical exam and sometimes imaging to rule out other conditions.
- Management: Supportive care: supportive bras, warm compresses, dietary adjustments.
Tip: Use self-exams to track patterns and discuss persistent changes with your healthcare provider, supporting breast wellness.
4. Nipple Discharge
- Normal vs. Concerning: Clear or milky discharge may be normal; spontaneous, bloody, or colored discharge requires evaluation.
- Possible Causes: Infection, duct ectasia, benign papilloma, or rarely cancer.
- Management: Medical evaluation to determine cause; imaging or lab tests may be required.
Tip: Keep track of discharge appearance, frequency, and triggers for proper breast health monitoring.
5. Skin and Tissue Changes
- Symptoms to Watch For:
- Dimpling, puckering, or redness
- Thickening or swelling of the breast
- Changes in nipple shape or inversion
- Possible Causes: Infection, inflammation, benign growths, or malignancy.
Tip: Report sudden or persistent changes to a healthcare provider immediately to protect your breast health.
6. Key Takeaways
- Most breast lumps and changes are benign, but monitoring breast health is crucial.
- Perform regular self-exams and maintain screening schedules to support healthy breasts.
- Keep a breast health journal to track any changes and share them with your doctor, improving overall breast wellness.
Lifestyle and Diet for Healthy Breasts

Maintaining healthy habits can significantly support breast health, lower disease risk, and complement regular screenings. Lifestyle choices affect hormone balance, tissue health, and overall well-being.
@@@@@@@@@@@2/2
1. Nutrition for Breast Health
Fruits and Vegetables: Rich in antioxidants like vitamins C and E, which protect breast tissue.
Whole Grains and Fiber: Helps regulate estrogen levels, supporting hormonal balance.
Healthy Fats: Include omega-3 fatty acids (salmon, walnuts, flaxseeds) for anti-inflammatory benefits.
Limit Processed Foods and Sugar: High sugar and trans fats may increase cancer risk and inflammation.
Tip: A colorful plate with vegetables, fruits, lean proteins, and whole grains supports both breast and overall health.
2. Exercise and Physical Activity
Recommended Activity: At least 150 minutes of moderate exercise per week (walking, swimming, cycling) or 75 minutes of vigorous activity.
Strength Training: Two sessions per week improve muscle tone and overall metabolic health.
Benefits for Breast Health: Helps maintain healthy weight, reduce estrogen-related risk, and improve lymphatic circulation.
Tip: Include a mix of cardio, strength, and flexibility exercises for optimal wellness.
3. Weight Management
Maintaining a healthy BMI reduces risk of breast cancer, especially post-menopause.
Excess body fat increases estrogen, which can stimulate breast tissue growth.
Tip: Small, sustainable lifestyle changes—like walking 30 minutes daily and mindful eating—are more effective long-term than extreme diets.
4. Limiting Alcohol and Tobacco
Alcohol: Even moderate intake increases breast cancer risk.
Tobacco: Smoking damages DNA and increases risk of breast and other cancers.
Tip: Limit alcohol to 1 drink per day or less, and avoid tobacco entirely.
5. Stress Management and Sleep
Chronic stress can disrupt hormones and immune function.
Ensure you get between 7 and 9 hours of restorative sleep every night
Stress-reducing activities: yoga, meditation, deep breathing, or journaling.
Tip: Healthy mental habits support both hormone balance and overall breast wellness.
6. Environmental and Lifestyle Awareness
Limit exposure to endocrine disruptors in plastics, cosmetics, and cleaning products.
Wear properly fitting bras to reduce tissue strain and maintain comfort.
Be mindful of posture and ergonomics, especially during long hours sitting at work.
Tip: Simple lifestyle adjustments can reduce long-term risks and support breast tissue health.
7. Key Takeaways
Nutrition, exercise, weight management, and stress control are all pillars of breast wellness.
Small, consistent habits have a compounded positive effect over time.
Combine lifestyle practices with self-exams and regular screenings for maximum protection.
Well-Woman Care Beyond Breasts

Breast health is just one aspect of overall well-woman care. A holistic approach includes hormonal health, reproductive wellness, and mental well-being, ensuring women maintain optimal health throughout life.
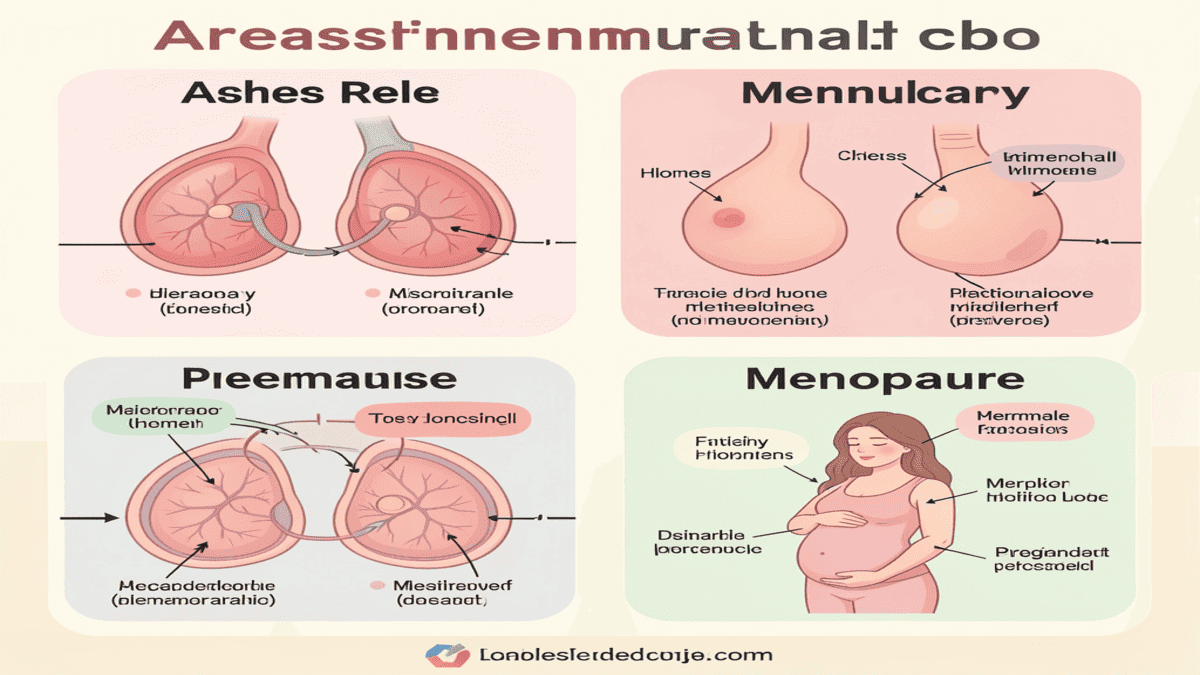
1. Hormonal Health
Menstrual Health: Track cycles to monitor irregularities, pain, or heavy bleeding.
Menopause: Watch for hot flashes, mood changes, and changes in breast tissue.
Hormone Replacement Therapy (HRT): Discuss risks and benefits with your doctor if needed.
Tip: Regular check-ins with a healthcare provider help manage hormonal changes safely.
2. Reproductive Health
Regular Gynecological Exams: Includes Pap smears, STI screenings, and pelvic exams.
Fertility Awareness: Understanding your cycle helps with family planning or identifying abnormalities.
Pregnancy and Postpartum Care: Monitor breast and reproductive health before, during, and after pregnancy.
Tip: Keep a reproductive health calendar to track exams, vaccinations, and fertility indicators.
3. Mental and Emotional Wellness
Chronic stress can disrupt hormones, sleep, and immune function.
Mindfulness, meditation, and therapy can improve overall well-being.
Social support networks, hobbies, and self-care routines contribute to emotional health.
Tip: Integrate mental wellness practices into daily routines—short meditation sessions, journaling, or nature walks.
4. Preventive Care
Vaccinations: Stay up-to-date on recommended vaccines (HPV, flu, etc.).
Bone Health: Calcium, vitamin D, and weight-bearing exercises help prevent osteoporosis.
Cardiovascular Health: Blood pressure, cholesterol, and glucose checks are important at all ages.
Tip: Preventive care is most effective when combined with regular screenings and healthy lifestyle choices.
5. Lifestyle Integration
Combine diet, exercise, stress management, and preventive care for overall wellness.
Educate yourself on risk factors and early warning signs for chronic diseases.
Make holistic health a routine, not an occasional focus.
Tip: Use a well-woman wellness checklist to track appointments, screenings, and lifestyle habits.
6. Key Takeaways
Well-woman care goes beyond breast health, encompassing hormonal, reproductive, and mental health.
Preventive care and lifestyle habits are essential for long-term wellness.
Integrating self-awareness, regular check-ups, and holistic practices ensures women stay healthy in 2026 and beyond.
When to See a Doctor
Even though many breast changes are normal, some symptoms require prompt medical evaluation. Early consultation can ensure proper diagnosis and effective treatment.
1. New Lumps or Thickening
What to look for: Any new lump, firm area, or thickened tissue in your breast or underarm.
Why it matters: While many lumps are benign, new or rapidly growing lumps should be checked to rule out cancer.
Action: Schedule a clinical breast exam and possible imaging (ultrasound or mammogram).
2. Persistent Pain or Tenderness
Normal vs. Concerning: Mild tenderness before your period is normal, but ongoing or worsening pain is not.
Possible Causes: Infection, cysts, inflammation, or rarely malignancy.
Action: Track the pain, note its location, and consult your healthcare provider if it persists beyond your menstrual cycle.
3. Skin Dimpling or Nipple Changes
Red Flags:
Skin puckering, dimpling, or thickening
Nipple inversion (if new)
Redness, rash, or swelling
Why it matters: These may indicate underlying changes, including inflammatory breast conditions or cancer.
Action: Prompt evaluation by a doctor is essential for early detection.
4. Nipple Discharge
Concerning Discharge: Spontaneous, bloody, or clear discharge from one nipple.
Possible Causes: Duct papilloma, infection, or rarely cancer.
Action: Document the discharge (color, frequency) and seek medical assessment.
5. Family History and Genetic Risk
High-Risk Factors:
First-degree relative with breast or ovarian cancer
Known BRCA1/BRCA2 or other cancer-related gene mutations
Personal history of breast abnormalities
Action: Discuss personalized screening schedules and genetic counseling with your healthcare provider.
6. Key Takeaways
Early evaluation of any unusual breast changes improves outcomes.
Track symptoms, family history, and breast changes to provide detailed information to your doctor.
Combining self-awareness, screenings, and timely consultation is the most effective approach to breast health.
Prevention and Risk Reduction

While some risk factors like genetics can’t be changed, there are many steps women can take to actively reduce their risk of breast disease and support overall well-woman health.
1. Maintain a Healthy Weight and Active Lifestyle
Why it matters: Excess body fat increases estrogen levels, which can stimulate breast tissue and raise the risk of breast cancer.
How to achieve it:
Aim for 150 minutes of moderate exercise weekly or 75 minutes of vigorous activity.
Include strength training 2 times per week to support metabolism and overall health.
Prioritize eating a well-balanced diet full of whole grains, fruits, vegetables, and lean meats.
Tip: Consistent, moderate changes are more sustainable than extreme diets or workouts.
2. Follow Recommended Screening Schedules
Screenings save lives: Early detection through mammograms, ultrasounds, and clinical breast exams improves outcomes.
Guidelines for average-risk women:
Mammograms starting at age 40, every 1–2 years
Clinical breast exams per healthcare provider recommendations
High-risk women: May need earlier or more frequent screenings and genetic counseling.
Tip: Keep a personal health calendar to track exams and follow-up appointments.
3. Educate Yourself and Loved Ones
Learn the warning signs of breast changes: new lumps, skin changes, nipple discharge, or persistent pain.
Share knowledge with family and friends to increase awareness and encourage preventive practices.
Awareness helps detect changes earlier, leading to better outcomes.
Tip: Use checklists, apps, or journals to track symptoms and educate others.
4. Avoid Prolonged Exposure to Risk Factors
Alcohol: Limit to 1 drink per day or less, as even moderate intake increases risk.
Tobacco: Avoid smoking entirely, as it damages DNA and elevates cancer risk.
Environmental Hazards: Reduce exposure to endocrine disruptors found in certain plastics, cosmetics, and chemicals.
Tip: Small lifestyle changes, like quitting smoking or reducing alcohol, have long-term protective effects.
5. Key Takeaways
Risk reduction combines healthy lifestyle, awareness, and regular screening.
Even small, consistent actions—like daily walks, mindful eating, or scheduling exams—can significantly lower risk.
Prevention is most effective when integrated into holistic well-woman care.

Conclusion
Breast health is a lifelong commitment and a vital part of well-woman care. By performing regular self-exams, scheduling screenings, adopting a healthy lifestyle, and being aware of risk factors, women can take control of their wellness in 2026 and beyond. Prioritize your breasts as part of your overall health strategy—your future self will thank you.
Frequently Asked Questions (FAQ)
1. How frequently should I examine my breasts?
Women are advised to perform a monthly self-exam, ideally a few days after their period when breasts are less tender.
Becoming familiar with your normal breast tissue helps detect changes early.
2. At what age should I start mammograms?
Average-risk women: Start at age 40 and continue every 1–2 years.
High-risk women: May need earlier or more frequent screenings based on family history or genetic factors.
Consult a healthcare professional about your personal risk at all times.
3. What are the common signs of a breast problem?
New lumps or thickening
Persistent breast pain or tenderness
Nipple discharge (especially spontaneous or bloody)
Skin changes like dimpling, redness, or puckering
Nipple inversion (if it is a new change)
4. Are all breast lumps cancerous?
No. Most breast lumps are benign, such as cysts or fibroadenomas.
However, any new lump should be evaluated by a healthcare professional to rule out malignancy.
5. How can I reduce my risk of breast cancer?
Maintain a healthy weight and active lifestyle
Follow recommended screening schedules
Limit alcohol and avoid tobacco
Eat a diet rich in fruits, vegetables, and whole grains that is well-balanced.
Manage stress and get adequate sleep
6. Can lifestyle affect breast health?
Yes. Exercise, diet, stress management, and avoiding harmful substances all support breast tissue health and reduce disease risk.
Healthy habits complement regular screenings and medical care.
7. When should I see a doctor immediately?
If you notice:
A new lump or thickening
Persistent breast pain
Nipple discharge (spontaneous or bloody)
Skin dimpling, redness, or puckering
Also consider early consultation if you have a strong family history or known genetic risk.
8. Are there any natural ways to support breast health?
While no remedy can replace screenings or professional care, these practices may help:
Maintain a balanced, antioxidant-rich diet
Stay physically active
Limit alcohol and avoid tobacco
Manage stress and sleep well
9. How do genetics affect breast health?
Mutations in BRCA1, BRCA2, or other genes increase the risk of breast and ovarian cancers.
Women with strong family history may benefit from genetic counseling and personalized screening plans.
10. What is well-woman care?
Holistic care that includes:
Breast health
Hormonal and reproductive health
Preventive screenings (Pap smears, bone density, vaccines)
Mental and emotional wellness
Integrating all these aspects ensures optimal long-term health.
Disclaimer
This article should not be used as a replacement for expert medical advice; it is merely meant to be informative. Always consult a qualified healthcare provider regarding any breast health or well-woman care concerns.