Effective Fungal Acne Treatment at Home – 2025 Guide
What Is Fungal Acne? Why Fungal Acne Treatment at Home Is Often Misdiagnosed

Table of Contents
- Problem: What Is Fungal Acne — And Why It’s Often Mistaken
- Agitate: Why Fungal Acne Treatment at Home Matters
- Solution: How to Do Fungal Acne Treatment at Home Effectively
- Step 1: Confirm Fungal Acne Patterns
- Step 2: Anti-Fungal Cleanser / Body Wash
- Step 3: Topical Antifungal Treatment
- Step 4: Adjust Skincare + Lifestyle
- Step 5: Natural or Complementary Remedies
- Example Case Study: From Persistent Breakouts to Clearer Skin
- Why This Approach Works — The Science Behind Fungal Acne Treatment
- Common Mistakes to Avoid in Fungal Acne Treatment
- When to Consult a Physician (or Dermatologist)
- Summary — The Bottom Line on Fungal Acne Treatment at Home
- Final Thoughts
- FAQ: Fungal Acne Treatment at Home
Problem: What Is Fungal Acne and Why It’s Frequently Misdiagnosed
Fungal acne, medically called Malassezia folliculitis, is a skin condition that is frequently misdiagnosed as traditional acne. Unlike bacterial acne, which is caused by clogged pores and bacteria, fungal acne develops from an overgrowth of yeast (Malassezia) that naturally lives on the skin. This yeast normally exists in balance with the skin microbiome, but under certain conditions—such as humidity, excessive sweating, or the use of heavy oils—it can multiply and cause inflammation.
Key Symptoms of Fungal Acne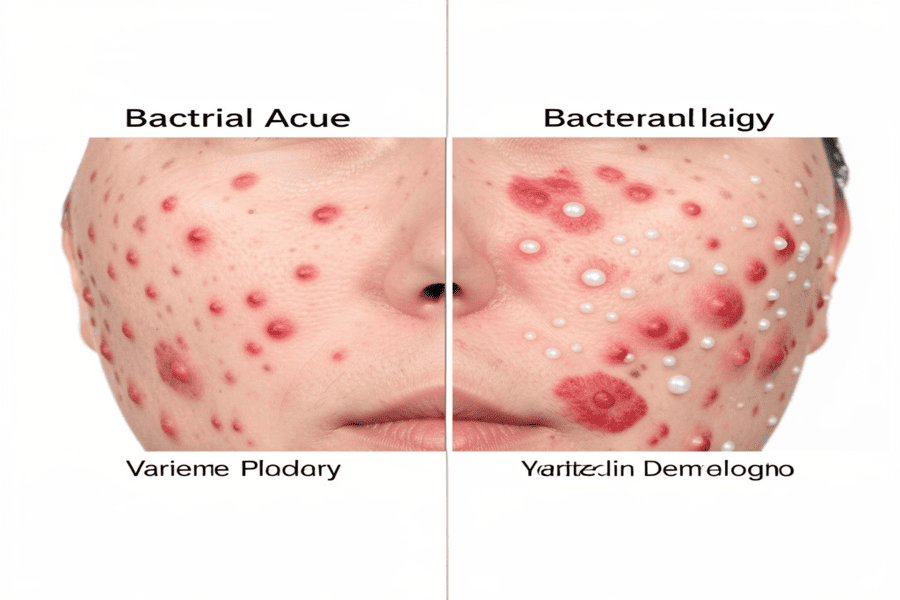
Recognizing fungal acne is crucial because it requires a different treatment approach than standard acne. Common signs include:
- Small, uniform bumps:Unlike typical acne, which varies in size and shape, fungal acne tends to appear as small, evenly sized pimples clustered together. These bumps are often itchy or slightly inflamed, which can cause discomfort.
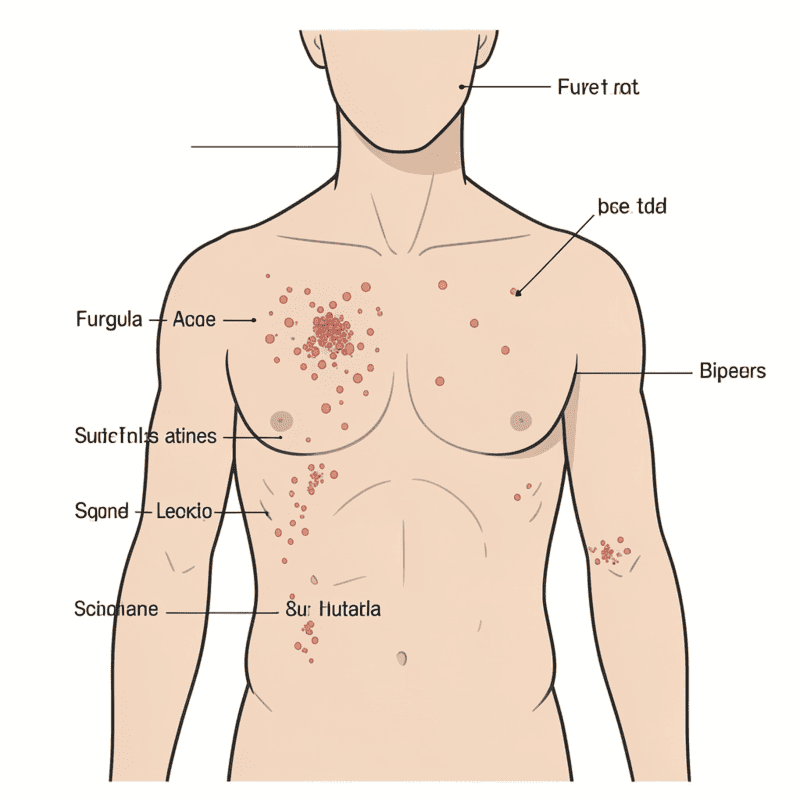
- Affected areas:Fungal acne usually appears on the chest, back, shoulders, neck, and upper arms. These are areas prone to sweat accumulation and friction, creating a warm environment where yeast thrives.
- Itching or burning sensation:One distinguishing feature is that the bumps can feel itchy, irritated, or even slightly burning (itchy skin). Traditional acne rarely causes such persistent itching.
- Resistance to common acne treatments:Many sufferers notice no improvement with antibiotics or benzoyl peroxide. In fact, these treatments may sometimes make the condition worse by disrupting the natural balance of skin microbes, allowing yeast to flourish.
Why Fungal Acne Treatment at Home Matters
Fungal acne can easily be mistaken for regular acne or even heat rashes and allergic reactions. Here’s why:
- Visual similarity:The small, red bumps look like typical pimples, so many people assume over-the-counter acne treatments will work.
- Failure of traditional treatments:Patients often try benzoyl peroxide, salicylic acid, or antibiotics for months. When these fail, frustration grows, and the underlying fungal cause is usually overlooked.
- Delayed diagnosis:In some studies, patients went years without proper treatment before a dermatologist identified fungal acne. This is partly because standard acne treatments are widely promoted, while fungal acne is less known outside dermatology circles.
Contributing Factors
Several environmental and lifestyle factors can trigger or worsen fungal acne:
- High humidity and sweating:Yeast thrives in warm, moist environments. People living in tropical climates or exercising frequently are more prone.
- Tight clothing:Synthetic fabrics or clothes that trap sweat can increase yeast growth on the chest and back.
- Oily skin products:Heavy lotions, creams, or oils can feed the yeast, worsening the condition.
- Disrupted skin microbiome:Overuse of antibacterial cleansers or harsh soaps can reduce beneficial bacteria, giving yeast an advantage.
Statistics and Clinical Evidence
Fungal acne is more common than many realize. In a study of 217 patients initially diagnosed with acne, approximately 25% actually had fungal acne (PubMed). This highlights how often fungal acne is overlooked and mismanaged, leading to:
- Extended discomfort
- Repeatedly unsuccessful treatments
- Emotional frustration due to persistent itchy skin
Signs You Might Have Fungal Acne
You may suspect fungal acne if:
- Bumps appear in clustersrather than randomly scattered
- Your skin itches or burns frequently
- Antibiotics or conventional acne treatments do not help
- The affected areas are common fungal acne zones: chest, back, shoulders, neck, or upper arms
Agitate:The Significance of Treating Fungal Acne at Home
Fungal acne may seem like “regular acne,” but treating it incorrectly can prolong discomfort, cause flare-ups, and even worsen the condition. Understanding why standard treatments often fail and why natural remedies aren’t always enough is essential for effective home care.
Standard Treatments Often Fail
One of the biggest challenges with fungal acne is that it does not respond to conventional acne treatments. Most acne products, like antibiotics, benzoyl peroxide, or salicylic acid, target bacterial causes of acne, not yeast. Using these products can sometimes backfire:
- Disrupts the skin microbiome:Antibiotics or harsh acne washes reduce beneficial bacteria, giving Malassezia yeast more room to grow.
- Worsens inflammation:Over-drying or irritating the skin can trigger flare-ups and persistent itchy skin.
- False reassurance:People may believe their acne will improve, wasting weeks or months on ineffective treatments.
Clinical evidence:
- A study showed that 65% of fungal acne patientshad previously tried standard acne treatments without improvement.
- Only 12% of cases resolved with topical antifungal creams alone, underscoring the necessity of a regimented at-home regimen that combines antifungal therapy with lifestyle modifications.
Recurrence Is Common
Even after initial improvement, fungal acne tends to recur if underlying triggers aren’t addressed. This is why home treatment must go beyond creams and cleansers. Common recurrence factors include:
- Humidity:Warm, moist environments encourage yeast proliferation. Tropical climates or excessive indoor heating can exacerbate flare-ups.
- Sweat:Physical activity, workouts, or sweating under tight clothing creates an ideal environment for yeast.
- Tight or synthetic clothing:Traps heat and moisture, leading to increased yeast growth on the chest and back.
- Oils and heavy creams:Oil-based moisturizers, hair oils, or thick lotions can feed the yeast.
- Hygiene habits:Infrequent showers, sleeping in sweaty clothes, or not washing workout gear increases the risk of recurrence.
Even patients who successfully clear fungal acne can relapse if these factors aren’t managed, emphasizing the importance of a holistic home treatment approach.
Natural Remedies Can Mislead
Many sufferers turn to online advice, searching for “natural cures for fungal acne”. Common suggestions include:
- Antifungal extract derived from plants
- diluted acidic skin solutionr
- Masks made of raw honey
- Turmeric or botanical remedies
While some ingredients may have mild antifungal properties, evidence is limited. Over-reliance on these remedies can:
- May trigger skin sensitivity or discomfort
- Worsen fungal acneif applied improperly
- Delay the use of effective antifungal treatments
Pro Tip: Natural remedies should complement, not replace, evidence-based antifungal treatments. They can be used in moderation alongside proper cleansers, creams, and lifestyle adjustments.
Why Home Treatment Must Be Structured
Because fungal acne is stubborn and easily recurrent, a structured home treatment routine is essential. This includes:
- Targeted antifungal cleansers and creams
- Lifestyle adjustmentsto prevent yeast overgrowth
- Maintenance routineseven after clearing
- Supportive natural remediesif desired
Without this structured approach, fungal acne can linger for months or even years, causing discomfort, self-consciousness, and repeated failed attempts with standard acne products.
Solution: How to Effectively Treat Fungal Acne at Home
Fungal acne can be stubborn, but home treatment is possible with a structured and consistent routine. The goal is to reduce yeast overgrowth, soothe irritation, and prevent recurrence. Below is a step-by-step guide based on dermatology research and practical experience.
Step 1: Confirm Fungal Acne Patterns
Before starting treatment, make sure your breakouts are likely fungal acne. Misdiagnosis is common, and treating bacterial acne with antifungals or vice versa can delay results.
Look for tell-tale signs:
- Uniform, clustered bumpson the chest, back, shoulders, or neck. Unlike bacterial acne, the bumps are often the same size and appear in groups.
- Persistent itchy skinthat doesn’t respond to standard acne creams.
- No improvement with antibioticsor benzoyl peroxide after several weeks.
Tip: If unsure, a dermatologist can examine a skin sample under a microscope to confirm Malassezia yeast. Early confirmation can save months of ineffective treatment.
Step 2: Anti-Fungal Cleanser / Body Wash

Proper cleansing is the first line of defense. Reducing yeast on the skin and in hair follicles helps prevent further infection.
Recommended cleansing steps:
- Use a fragrance-free, non-comedogenic cleansersuch as Cetaphil to avoid irritation.
- Anti-dandruff shampooscontaining ketoconazole, selenium sulfide, or zinc pyrithione can double as a body wash to target fungal acne on the chest, back, and shoulders.
- Before rinsing, let the product lather on the afflicted areas forthree to five minutes.
Repeat daily or every other day depending on severity.
Why this works:
These shampoos reduce yeast load and soothe inflammation without over-drying the skin. Avoid harsh soaps or scrubs, which can disrupt the skin microbiome and worsen itchy skin.
Step 3: Topical Antifungal Treatment

Once yeast overgrowth is established, topical antifungal creams are key to clearing fungal acne.
Application guidelines:
- Use creams or ointments containing ketoconazoleor clotrimazole.
- For two to four weeks, apply twice a day to the afflicted areas.
- Continue the treatment even if bumps improve early. Stopping too soon may allow yeast to rebound.
Pro Tip:
- For stubborn cases, combine the topical treatment with your antifungal body wash for maximum effect.
- Avoid mixing with oil-based moisturizers, as oils can feed yeast.
Step 4: Adjust Skincare + Lifestyle
Fungal acne is highly influenced by environmental and lifestyle factors, so adjusting daily habits is crucial.
Lifestyle adjustments include:
- Loose, breathable clothing:Cotton or moisture-wicking fabrics reduce heat and sweat accumulation.
- Shower and change clothes after sweating:Prevents yeast from thriving in warm, damp conditions.
- Avoid oil-based moisturizers, which can worsen fungal acne. Use non-comedogenic, lightweight productsinstead.
- Maintain a weekly antifungal cleansing routine, even after the skin clears, to prevent recurrence.
Extra Tip: Keep workout gear and bedding clean. Tight or synthetic fabrics that retain sweat can trigger flare-ups.
Step 5: Natural or Complementary Remedies
Some natural ingredients can complement treatment, though they should never replace antifungal therapy.
Supportive options include:
- Tea Tree Oil (diluted):Mild antifungal effect; can be applied with a carrier oil.
- Apple cider vinegar:Can help restore skin pH; always dilute before use.
- Honey masks:Raw honey has antimicrobial properties; patch-test first.
Tip: Apply natural remedies sparingly. Overuse can irritate sensitive skin and worsen fungal acne. Treat them as supplementary, not primary treatment.
Step 6: Monitor Progress and Maintenance
Even after visible improvement, fungal acne can return. Effective home management includes:
- Tracking bump count and itchinessweekly
- Continuing antifungal cleansingonce or twice per week for maintenance
- Maintaining a light, oil-free skincare routine
- Observing triggers like heat, sweat, or new skincare products
Key Takeaway: Consistency over several weeks is essential. Most patients notice significant improvement within 2–4 weeks, and complete clearance may take 4–6 weeks.
An Example Case Study: Transitioning from Chronic Pimples to Clearer Skin

Background
A 24-year-old adult experienced persistent acne-like bumps on the back, chest, and shoulders for eight months. The breakouts were itchy, sometimes burning, and resistant to multiple conventional treatments, including
- Washes with benzoyl peroxide
- Serums containing salicylic acid
- Antibiotics available over-the-counter
Despite these efforts, the bumps worsened after a few weeks, leaving the skin inflamed and sensitive. The patient reported frustration and embarrassment due to visible clustered pimples and constant itching itchy skin.
Diagnosis Shift
After a detailed examination, a dermatologist suspected fungal acne (Malassezia folliculitis). A skin scraping under a microscope confirmed abundant Malassezia spores, the yeast responsible for fungal acne.
Key point: Misdiagnosis is common. Research shows that 25% of patients who were initially diagnosed with acne actually have fungal acne PubMed.
Once diagnosed, a structured home treatment plan was implemented to target the yeast and prevent recurrence.
Treatment Plan
The patient followed a step-by-step home regimen designed to reduce fungal growth, soothe irritation, and adjust lifestyle habits:
- Shampoo with ketoconazole as a body wash
- Applied to affected areas (back, chest, shoulders) every other day, left on for 3–5 minutes before rinsing.
- Reduced the fungal load and calmed inflammation.
- Topical use of ketoconazole cream
- Applied twice daily on affected patches.
- Continued for four weeks, even after a discernible improvement, to prevent relapse.
- Non-comedogenic moisturizer
- Lightweight, oil-free moisturizer applied sparingly to prevent dryness without feeding yeast.
- Helped reduce irritation from antifungal products.
- Lifestyle adjustments
- Wore loose cotton clothing and avoided tight synthetic fabrics.
- Showered and changed clothes promptly after workouts.
- Reduced exposure to excessive sweat and humidity.
- Optional supportive remedies
- Occasionally applied diluted tea tree oil for mild antifungal support.
- Followed patch-test guidelines to avoid irritation.
Outcome (4 Weeks)
Week 1:
- Itchiness and burning sensations significantly decreased.
- Skin felt calmer, less inflamed, and more comfortable.
Week 2:
- Early reduction in visible bumps.
- less newly formed lesions.
Week 3-4:
- Bumps are reduced by about 60–70%.
- Skin appeared smoother, less red, and less irritated.
- The patient reported feeling more at ease and confident.
6 Weeks (Follow-Up):
- No new breakouts observed.
- Maintained lifestyle changes and weekly antifungal cleansing.
- Patient continued light moisturizer use and avoided oil-based creams to prevent relapse.
Key Lessons From This Case
- Structured home treatment works:Combining antifungal cleansers, topical creams, and lifestyle adjustments yielded visible results within 4 weeks.
- Early diagnosis is critical:Identifying Malassezia as the cause prevented months of ineffective treatments.
- Lifestyle habits are essential:Loose clothing, proper showering routines, and avoiding heavy oils were crucial to maintaining clear skin.
- Maintenance prevents recurrence:Weekly antifungal washes and consistent skincare ensured long-term success.
Understanding the Science Behind Home Treatment for Fungal Acne
Understanding why structured home treatment works helps explain why traditional acne methods often fail. The approach targets both the biological cause and environmental triggers that allow fungal acne to persist.
Targets the Root Cause
Fungal acne develops due to an overgrowth of Malassezia yeast, which naturally lives on the skin. Unlike bacterial acne, standard antibiotics and benzoyl peroxide do not affect yeast, which is why they often fail.
- Topical antifungal creams(ketoconazole, clotrimazole) inhibit yeast growth directly, reducing bumps and irritation.
- Anti-dandruff shampooscontaining selenium sulfide or zinc pyrithione applied to affected areas can also suppress Malassezia in hair follicles.
Scientific insight: Studies show that even short-term yeast overgrowth can trigger persistent inflammation. Targeting the fungus early reduces immune response and prevents chronic flare-ups.
Alters the Skin Environment
Malassezia thrives in warm, moist, and oily environments. Lifestyle and skincare adjustments make your skin less hospitable to yeast:
- Wearing loose, breathable clothingprevents sweat accumulation.
- Showering promptly after workouts removes excess yeast and sweat.
- Avoiding oil-based or comedogenic productsdenies the yeast its nutrient source.
By changing the skin environment, fungal acne treatment at home becomes more effective and long-lasting.
Sufficient Treatment Duration
Fungal acne requires patience and consistency. Even if bumps improve quickly, the yeast can rebound if treatment is too short.
- Topical antifungalsshould be applied 2–4 weeks consistently.
- Follow-up maintenance washesonce or twice weekly can prevent recurrence.
This explains why many home remedies or short-term treatments fail—without sufficient duration, the yeast returns.
Common Mistakes in Fungal Acne Treatment at Home
Even with the right knowledge, many people make mistakes that undermine fungal acne treatment at home. Avoid the following pitfalls:
- Using oil-based creams:Heavy moisturizers feed Malassezia and worsen breakouts.
- Stopping antifungal treatment too early:Partial improvement may feel like success, but the yeast can rebound.
- Assuming all pimples are bacterial acne:Misdiagnosis leads to ineffective treatments.
- Relying solely on natural remedies:Tea tree oil, honey, or apple cider vinegar are supportive, not primary treatments.
- Ignoring lifestyle triggers:Sweat, tight clothing, and poor hygiene sustain yeast-friendly environments.
Pro Tip: Pair antifungal treatments with consistent lifestyle adjustments for long-term relief.
When to Consult a Physician (or Dermatologist)
While most mild-to-moderate fungal acne can be treated at home, consult a dermatologist if:
- After four to six weeks of regular at-home therapy, there was no improvement.
- Breakouts are widespread, painful, or rapidly spreading.
- Complicating factors exist, such as immune suppression or skin barrier issues.
Why professional care matters: Severe or persistent cases may require oral antifungals or tailored medical intervention to prevent scarring and chronic infection.
Summary — Bottom Line on Fungal Acne Treatment at Home
Effective fungal acne treatment at home involves a combination of targeted antifungal therapy, lifestyle adjustments, and patience. The key steps:
- Antifungal cleansers: Anti-dandruff shampoos or non-comedogenic cleansers reduce yeast load.
- Topical antifungal creams: Apply ketoconazole or clotrimazole consistently for 2–4 weeks.
- Lifestyle adjustments: Wear loose clothing, shower after sweat, and avoid oils.
- Minimalistic skincare: Stick to lightweight, non-comedogenic products.
- Patience and maintenance: Results take 2–4 weeks; continue preventive routines to reduce recurrence.
Key takeaway: Fungal acne is manageable at home if you focus on root cause treatment and consistent care.
Final Thoughts
Fungal acne can feel frustrating, but a structured approach at home works. Avoid chasing trendy products or overcomplicated routines. Focus on:
- Topical antifungal treatments, including creams and cleansers
- Modifications to lifestyle and hygiene
- Consistent, minimalistic skincare
With diligence and patience, most people see significant improvement within 4–6 weeks. Long-term maintenance ensures your skin stays clear, calm, and resilient.
FAQ: Fungal Acne Treatment at Home
Q1: How fast will I see results with fungal acne treatment at home?
With consistent care, most people notice improvements in stages:
- Itch reduction:Often within 1 week of starting antifungal cleansers and creams.
- Visible bump improvement:Typically 2–4 weeks, depending on severity and adherence to treatment.
- Full clearance:Can take 4–6 weeks; maintenance routines help prevent relapse.
Tip: Track your progress weekly by photographing affected areas—this helps you see subtle improvements you might not notice day-to-day.
Q2: Is fungal acne contagious?
No. Fungal acne (Malassezia folliculitis) develops from yeast that naturally exists on your skin.
- It is not spread by touchlike bacterial infections.
- However, shared items that trap sweat and heat, like towels or tight clothing, can indirectly create environments that promote yeast growth.
Tip: Keep workout gear and towels clean, and practice proper hygiene to reduce flare-ups.
Q3: Can I use my regular moisturizers during treatment?
- Avoid oil-based or heavy creams, as they feed Malassezia yeast.
- Use lightweight, non-comedogenic productsinstead.
- Applying a thin layer of Weleda Skin Food Lightor similar product can hydrate the skin without worsening fungal acne.
Tip: Stick to minimalistic skincare routines while actively treating fungal acne.
Q4: Are natural remedies effective for fungal acne?
Some natural ingredients can provide supportive effects:
- Tea tree oil (carrier oil diluted)
- Apple cider vinegar diluted with water
Honey masks (raw honey, patch-tested first)
Important: Natural remedies are never a replacement for antifungal creams or proper cleansers. Overuse or improper application may irritate the skin and worsen fungal acne.
Tip: Use natural remedies sparingly and only as an adjunct to structured home treatment.
Q5: Do I need oral antifungals?
Oral antifungals are usually unnecessary for mild-to-moderate fungal acne. They may be prescribed if:
- The infection is severe, widespread, or persistent.
- Topical treatments and lifestyle adjustments have failed after 4–6 weeks.
Tip: Always consult a dermatologist before starting oral antifungals, as dosage and duration require medical supervision.
Q6: How can I prevent fungal acne from coming back?
Prevention focuses on controlling triggers:
- Shower and change clothespromptly after sweating.
- Wear loose, breathable fabricsto reduce heat and moisture.
- Maintain a weekly antifungal cleansing routine, even after the skin clears.
Additional Tips:
- Avoid heavy or oil-rich skincare products.
- Keep bedding, towels, and workout clothes clean.
- Limit exposure to extreme humidity or prolonged heat when possible.
Following these habits consistently ensures that fungal acne treatment at home remains effective and reduces the risk of recurrence.






9 Comments