Toasted Skin Syndrome Explained: Symptoms & Care
Toasted Skin Syndrome: Causes, Treatment, and Prevention (Erythema Ab Igne Explained)
Table of Contents
- Introduction
- What Is Toasted Skin Syndrome?
- Toasted Skin Syndrome Causes: How Heat Affects Your Skin
- Symptoms to Watch For
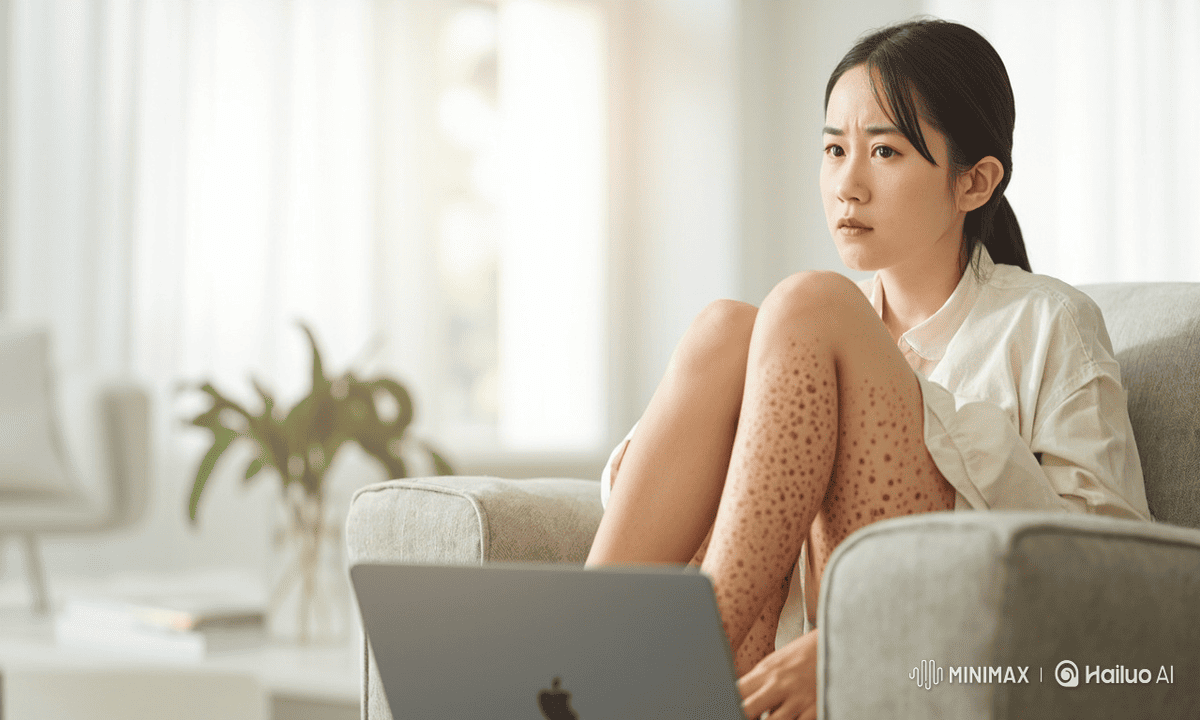
- Case Study: Real-Life Example of TSS
- Toasted Skin Syndrome Treatment: What Works
- Erythema Ab Igneous Prevention: Tips to Protect Your Skin
- When to See a Dermatologist
- Final Thoughts
- References
Introduction
Toasted Skin Syndrome is a skin condition caused by prolonged exposure to heat, often resulting in reddish-brown patches in a net-like pattern. Also known as Erythema Ab Igne, this condition develops gradually and can affect adults of all ages, especially those frequently using heating pads, laptops, or space heaters. Understanding its causes, symptoms, and treatment options is essential to prevent permanent skin discoloration and maintain healthy skin.
What Is Toasted Skin Syndrome?
Toasted Skin Syndrome (TSS), medically known as Erythema Ab Igne (EAI), is a skin condition caused by repeated or prolonged exposure to moderate heat. Unlike a typical burn, which occurs suddenly and is often painful, Toasted Skin Syndrome develops gradually, making it easy to overlook in the early stages. The condition manifests as reddish-brown or hyperpigmented patches, often arranged in a net-like or reticulated pattern. Over weeks or months, these patches may become more pronounced and can persist even after the heat source is removed.
Who Is at Risk for Toasted Skin Syndrome?
While Toasted Skin Syndrome can technically affect anyone, certain groups are more prone to developing the condition:
- Adults over 40: Aging skin is more sensitive to repeated heat exposure. The natural slowing of skin regeneration makes it easier for Toasted Skin Syndrome pigmentation to become permanent.
- Younger adults with lifestyle exposure: People who spend long hours using laptops on their laps or frequently sit near heaters may develop Toasted Skin Syndrome even in their 20s or 30s.
- Individuals with chronic pain: Those using heating pads or electric blankets daily for conditions like back pain or muscle stiffness may unknowingly expose their skin to heat that causes Toasted Skin Syndrome.
Common Areas Affected by Toasted Skin Syndrome
Toasted Skin Syndrome typically occurs on areas of the body directly exposed to heat. The most common sites include:
- Lower back: Especially for people using heating pads to relieve back pain.
- Thighs: Frequent exposure occurs when laptops are placed directly on laps.
- Arms: Exposure from hand warmers or space heaters.
- Abdomen or chest: Individuals using hot water bottles or heating pads in bed.
The condition rarely spreads beyond the area of direct heat contact, which helps differentiate Toasted Skin Syndrome from other skin conditions like eczema or generalized rashes.
Common Heat Sources That Cause Toasted Skin Syndrome
Toasted Skin Syndrome (TSS) can be triggered by repeated exposure to even moderate heat. Some of the most common sources include:
- Laptops and tablets: Placing devices on the lap for hours without a cooling pad can generate enough heat to contribute to Toasted Skin Syndrome over time.
- Space heaters and heated chairs: Sitting close to heaters or using heated seats for extended periods is a frequent cause of Toasted Skin Syndrome.
- Heating pads and electric blankets: Often used for chronic pain relief or warmth, prolonged use—even on low or medium settings—can lead to Toasted Skin Syndrome.
- Car heaters: People who sit near car heating vents in winter may notice early signs of Toasted Skin Syndrome, commonly on the lower back or thighs.
How Toasted Skin Syndrome Develops
The development of Toasted Skin Syndrome is gradual, which is why it often goes unnoticed in the early stages. Here’s what happens at the skin level:
- Initial capillary dilation: Repeated heat exposure causes small blood vessels in the skin to expand, creating temporary redness.
- Pigment deposition: Over time, melanocytes deposit excess pigment in the affected area, resulting in the brownish patches characteristic of Toasted Skin Syndrome.
- Cellular changes: Prolonged heat exposure damages skin cells, causing mild changes in texture and sometimes slight thickening of the skin.
Potential Risks of Toasted Skin Syndrome
Although Toasted Skin Syndrome is usually considered a cosmetic concern, it is not entirely harmless:
- The condition can persist for months or even years if heat exposure continues.
- Skin discoloration may remain even after the heat source is removed.
- Rarely, chronic Toasted Skin Syndrome has been associated with an increased risk of skin cancer, particularly squamous cell carcinoma, due to long-term cellular changes caused by heat damage.
Why Awareness Is Important
TSS is often underdiagnosed because:
- Early stages are painless and subtle.
- Pigmentation can be mistaken for a simple tan or skin blemish.
- Many individuals continue repeated heat exposure, thinking the skin changes are harmless.
Understanding what TSS looks like and identifying the heat source early is crucial to prevent long-term skin damage and pigmentation. Early recognition allows for simple interventions, such as removing the heat source and monitoring skin changes, which often leads to partial or full recovery.
Toasted Skin Syndrome Causes: How Heat Affects Your Skin
Understanding the causes of Toasted Skin Syndrome (TSS) is essential for both prevention and early intervention. TSS is not caused by accidental burns or chemical irritation—it develops gradually due to chronic, low-level heat exposure. Over time, this exposure damages the skin’s structure and pigmentation, creating the characteristic reddish-brown, net-like patches.
Prolonged Heat Exposure
The primary cause of TSS is repeated or prolonged exposure to moderate heat. Even if the heat does not feel intense or painful, consistent exposure over weeks or months can trigger changes in skin appearance. Common sources of heat include:
- Laptop use: Many people place laptops directly on their laps for hours at a time. The heat generated by the device—especially gaming laptops or high-performance machines—can gradually damage the skin.
- Heating pads: Frequently used for back pain, muscle soreness, or menstrual cramps, heating pads are a common trigger. Prolonged daily use can lead to pigmentation changes.
- Electric blankets: During cold months, prolonged contact with an electric blanket can expose the skin to low-level heat over several hours while sleeping.
- Car heaters and heated seats: Sitting close to car vents or using heated seats for long winter commutes can contribute to TSS, particularly on the lower back or thighs.
Other, less obvious heat sources may include hand warmers, hot water bottles, and infrared therapy devices. The key factor is duration and frequency: even moderate heat can cause damage if exposure is repeated consistently.
How Heat Damages Skin
Even though TSS does not cause immediate pain like a burn, chronic heat exposure leads to gradual structural and pigmentary changes in the skin. Here’s how the process unfolds:
- Capillaries Dilate
- When skin is exposed to heat, the tiny blood vessels (capillaries) expand to dissipate heat.
- This dilation initially causes temporary redness that often goes unnoticed.
- Melanin Accumulates
- Over time, the heat stimulates melanocytes, the pigment-producing cells in the skin.
- This leads to brownish patches, which are often arranged in a reticulated or net-like pattern.
- The pigmentation may persist even after the heat source is removed, especially if exposure is prolonged.
- Cellular Damage Occurs
- Repeated heat exposure damages skin cells, altering collagen and elastin fibers, and sometimes causing slight thickening of the affected area.
- These changes are subtle at first but can become permanent with continued exposure.
Long-Term Effects
- Persistent Pigmentation: Once TSS develops, the discoloration can remain for months or even years if heat exposure continues.
- Texture Changes: Skin may feel slightly rougher or leathery in affected areas.
- Increased Cancer Risk: Rarely, chronic TSS has been linked to squamous cell carcinoma, particularly in cases with long-term heat exposure and persistent pigmentation.
Why Awareness Matters
Because TSS develops slowly and is often painless, it is frequently overlooked. Many people dismiss early signs as tanning, bruising, or simple skin discoloration. Recognizing the role of prolonged heat exposure is critical to preventing permanent pigmentation and other complications.
- Early identification allows for simple interventions, such as removing or limiting the heat source.
- Preventive measures—like using barriers between skin and heat sources or limiting exposure time—can stop TSS before it becomes visible.
Symptoms to Watch For
Recognizing Toasted Skin Syndrome (TSS) early is essential for preventing long-term skin changes. Because TSS develops gradually and is often painless, many people overlook the early signs, which can result in persistent pigmentation or more serious complications over time.
Key Symptoms
- Reddish or Brownish Patches
- The most characteristic feature of TSS is discolored patches of skin.
- These patches usually appear in a net-like (reticulated) pattern, resembling a subtle lattice across the affected area.
- Early on, the patches may be reddish, gradually turning brown as melanin accumulates with repeated heat exposure.
- Common locations include the lower back, thighs, arms, and abdomen, depending on the heat source.
- Rough or Altered Skin Texture
- In addition to pigmentation changes, the affected skin may feel slightly rougher or leathery compared to surrounding skin.
- This is due to chronic heat-induced changes in skin structure, including mild thickening and subtle alterations in collagen fibers.
- Minimal to No Pain
- Unlike burns or rashes, TSS is usually painless.
- There is generally no itching, swelling, or blistering, which is why many people fail to notice it in the early stages.
- Persistence and Potential Permanence
- If the heat source continues to be applied over weeks or months, the pigmentation may become permanent, and subtle textural changes can remain.
- Even after removing the heat source, discoloration may take several months to fade, and in some cases, it may never completely disappear.
Why Early Detection Matters
While TSS is mostly a cosmetic concern, prolonged cases carry additional risks:
- Chronic pigmentation changes may make the skin more vulnerable to sun damage.
- Rarely, persistent Erythema Ab Igne has been linked to squamous cell carcinoma, a type of skin cancer.
- Early detection allows for simple interventions, such as removing the heat source, using protective barriers, and monitoring skin changes, which can prevent progression and reduce long-term complications.
Early Warning Tips
- Look for discoloration in areas frequently exposed to heat, even if the skin feels normal otherwise.
- Pay attention to net-like patterns rather than random patches.
- Track any changes with photographs over weeks or months to identify progression.
By staying aware of these subtle early signs, individuals can take preventive steps before permanent skin changes occur.
Case Study: Real-Life Example of Toasted Skin Syndrome
Real-life examples of Toasted Skin Syndrome (TSS) help illustrate how seemingly harmless habits can lead to long-term skin changes. This case highlights the gradual onset, presentation, and management of TSS in an everyday scenario.
Patient Profile
- Age and Lifestyle: 45-year-old female, working from home, spending long hours seated at a desk.
- Heat Exposure: Used a heating pad on her lower back daily for 6 months to relieve chronic muscle tension.
- Medical History: No prior skin conditions, no history of burns, rashes, or allergies.
This profile represents a common demographic at risk for TSS—adults with routine, low-level heat exposure over extended periods.
Symptoms Observed
The patient presented with the following signs:
- Reddish-Brown Net-Like Patches
- Patches were primarily located on the lower back, directly where the heating pad made contact.
- The pattern was reticulated, forming a subtle lattice-like appearance characteristic of TSS.
- The pigmentation initially appeared faint but became more pronounced over months of continued exposure.
- Slightly Rough Skin Texture
- A mild thickening and roughness of the affected area was noted, consistent with chronic heat-induced changes in skin structure.
- Painless Presentation
- The patient reported no pain, itching, or discomfort, which is typical for TSS and often leads to delayed recognition.
Diagnosis
- The dermatologist diagnosed the patient with Erythema Ab Igne (Toasted Skin Syndrome) based on clinical appearance, history of heat exposure, and pattern of pigmentation.
- No further testing was required, as TSS is usually diagnosed clinically.
- The dermatologist also advised the patient to monitor for changes in the patches, such as thickening or irregularity, which could indicate complications.
Treatment and Outcome
- Cessation of Heat Exposure
- The patient was instructed to stop using the heating pad directly on the skin.
- A barrier (towel) was suggested if occasional heat use was necessary.
- Monitoring and Follow-Up
- Regular skin check-ups were recommended to observe pigmentation changes and rule out any malignant transformation.
- Progress Over Time
- After 3–6 months, the reddish-brown pigmentation gradually faded, though some residual discoloration remained.
- Skin texture normalized over time, but minor hyperpigmentation persisted, highlighting that early intervention is crucial to prevent permanent changes.
Key Takeaways from the Case
- Common lifestyle habits can trigger TSS: Daily use of heating pads, laptops, or prolonged exposure to heaters can lead to noticeable skin changes over months.
- Early recognition is important: Because TSS is usually painless, patients may ignore early signs. Observing subtle discoloration patterns is critical.
- Simple interventions are effective: Removing the heat source often leads to gradual improvement, but permanent pigmentation can occur if exposure continues.
- Follow-up is essential: Even after resolution, regular skin monitoring is recommended to prevent rare but serious complications like squamous cell carcinoma.
This case illustrates that TSS is not just a cosmetic concern; it is a preventable condition with proper awareness and minor lifestyle adjustments.
Toasted Skin Syndrome Treatment: What Works
While prevention is always the most effective approach to avoid Toasted Skin Syndrome (TSS), there are several treatment options available for those who already show signs of the condition. The goal of treatment is to reduce pigmentation, restore skin texture, and prevent long-term complications.
1. Stop Heat Exposure
The first and most important step in treating TSS is to eliminate the source of chronic heat.
- Immediate action: Remove or reduce direct contact with heat sources such as laptops, heating pads, electric blankets, or car heaters.
- Expected results: Most pigmentation will gradually fade over a few months once the skin is no longer exposed to continuous heat.
- Additional tips: If heat use is necessary, such as for back pain, use barriers like towels or limit exposure to short intervals (e.g., 15–30 minutes).
Early removal of the heat source is critical, as prolonged exposure can lead to permanent skin discoloration.
2. Topical Treatments
For more noticeable pigmentation, dermatologists may recommend topical creams to accelerate fading and improve skin appearance.
- Retinoid creams: Promote skin cell turnover and help reduce hyperpigmentation.
- Hydroquinone: Lightens dark patches by inhibiting melanin production.
- Usage tips: Consistent daily application over several weeks to months is usually required for visible results.
- Precautions: Always follow a dermatologist’s instructions, as improper use can cause irritation or sensitivity.
Topical therapy is most effective when combined with cessation of heat exposure, ensuring that the skin is no longer under stress.
3. Laser Therapy
For persistent or resistant pigmentation, laser treatments offer a more targeted approach.
- How it works: Laser energy is absorbed by melanin deposits in the skin, breaking them down and promoting even skin tone.
- Effectiveness: Clinical studies report improvement in over 80% of patients with resistant TSS pigmentation.
- Considerations: Multiple sessions may be required, and treatment should be performed by a qualified dermatologist or laser specialist to minimize risks.
Laser therapy is especially helpful for long-standing TSS cases where topical treatments alone are insufficient.
4. Skin Monitoring
Even after treatment, ongoing monitoring of affected areas is important.
- Rare risks: Chronic TSS may rarely develop into squamous cell carcinoma, particularly if pigmentation persists for years.
- Regular dermatology check-ups: Recommended for individuals with long-term discoloration or those with ongoing heat exposure.
- Self-monitoring: Watch for changes in color, texture, or size of the patches, and report any irregularities promptly.
Evidence-Based Insight
A study published in the Dermatology Online Journal found:
- 60% of patients experienced improvement in pigmentation after stopping heat exposure combined with topical therapy.
- Laser therapy showed significant improvement in over 80% of persistent cases, particularly for long-term discoloration resistant to creams.
These findings reinforce that early intervention, removal of heat, and targeted treatment are the most effective ways to manage TSS.
Key Takeaways
- Removing the heat source is the cornerstone of treatment.
- Topical treatments accelerate fading but require consistent use over time.
- Laser therapy offers an option for resistant pigmentation, with high success rates.
- Regular monitoring ensures that rare complications like skin cancer are detected early.
Erythema Ab Igneous Prevention: Tips to Protect Your Skin
Preventing Toasted Skin Syndrome (TSS), also known as Erythema Ab Igne, is far easier than treating it. Because TSS develops gradually and is often painless, many people unknowingly continue behaviors that put their skin at risk. By adopting a few simple preventive measures, you can protect your skin, avoid pigmentation, and reduce long-term complications.
1. Limit Direct Heat Contact
The most effective way to prevent TSS is to minimize prolonged exposure to heat sources.
- Use barriers: Place towels, clothing, or laptop cooling pads between your skin and heat sources such as laptops, heating pads, or car heaters. This reduces the intensity of heat reaching your skin.
- Change positions: Avoid placing laptops directly on your lap. Use a desk, table, or lap desk to create distance between the device and your skin.
- Limit exposure duration: Try to avoid continuous heat exposure exceeding 30 minutes at a time. Frequent breaks allow the skin to cool down and recover.
- Adjust settings: For heating pads or electric blankets, use low-temperature settings whenever possible. Even mild heat can trigger TSS if applied consistently.
2. Monitor Skin Changes
Early detection of TSS allows for simple interventions before pigmentation becomes permanent.
- Know the early signs: Red patches that gradually turn brown in a net-like pattern are the hallmark of TSS.
- Track changes over time: Take photos of areas exposed to heat weekly or monthly to monitor any new patches or progression of discoloration.
- Consult a dermatologist promptly: If patches persist after removing the heat source or if you notice changes in texture, color, or shape, seek professional advice. Early evaluation can prevent complications and provide guidance on treatments like topical creams or laser therapy.
3. Adjust Lifestyle Habits
Making small changes in daily routines can greatly reduce the risk of TSS.
- Alternate pain relief methods: If you use heat for back pain, muscle soreness, or cramps, try ice packs, stretching, or physiotherapy as alternatives to prolonged heat exposure.
- Protective clothing: Wear clothing layers over areas that might contact heaters, heating pads, or car vents. Even thin fabrics provide a barrier that reduces heat penetration.
- Education and awareness: Share information about TSS with family, friends, and coworkers, especially those who frequently use laptops on laps or heating pads. Many people are unaware that these common habits can lead to skin damage.
Extra Tips for Prevention
- Rotate heat sources: Avoid using the same heat source on the same area of skin every day.
- Cool-down breaks: After using a heating pad or laptop on your lap, allow the skin to rest and cool for at least 15–30 minutes.
- Sun protection: If TSS affects exposed areas, apply sunscreen. Pigmented patches are more sensitive to UV damage.
Why Prevention Matters
Because TSS is slow-developing and often painless, prevention is far superior to treatment. Once pigmentation becomes established, even topical treatments or laser therapy may not fully restore the skin. By limiting heat exposure, monitoring skin changes, and making small lifestyle adjustments, you can avoid TSS entirely and maintain healthy skin.
When to See a Dermatologist
While Toasted Skin Syndrome (TSS) is usually a cosmetic issue, there are situations where professional evaluation is essential. Early consultation can help prevent permanent skin changes and detect rare but serious complications, including skin cancer.
Situations That Require Professional Attention
- Pigmentation Does Not Fade
- After removing the heat source, mild discoloration often fades over weeks to months.
- If the reddish-brown patches persist beyond 3–6 months, it’s a signal to seek a dermatologist.
- Persistent pigmentation may require topical treatments or laser therapy to accelerate fading.
- Changes in Texture, Lumps, or Irregular Color
- Watch for any thickening, roughness, or raised areas within the discolored patches.
- Uneven or irregular pigmentation can indicate cellular changes that need professional evaluation.
- Any lumps, scaly patches, or ulcerations should be examined immediately, as these could be early signs of skin cancer, such as squamous cell carcinoma.
- Early Consultation for Peace of Mind
- Even if changes appear mild, early evaluation ensures proper diagnosis and prevents unnecessary anxiety.
- Dermatologists can differentiate TSS from other skin conditions like eczema, fungal infections, or sun damage.
- They can also recommend appropriate treatments tailored to your skin type and severity of pigmentation.
Additional Tips
- Document your skin changes: Take photos periodically to show the dermatologist the progression.
- Note heat exposure history: Inform your doctor about your daily habits, such as laptop use, heating pads, or car heaters, to help confirm a TSS diagnosis.
- Regular monitoring: If you have a history of chronic heat exposure, consider annual skin checks, even if TSS resolves, to ensure there are no late complications.
Key Takeaway:
If discoloration persists, changes in texture appear, or irregular pigmentation develops, don’t wait—schedule a dermatology consultation. Early detection and professional guidance are the most effective ways to manage TSS, prevent permanent skin changes, and rule out serious conditions like skin cancer.
Final Thoughts
Toasted Skin Syndrome is a condition that may appear harmless but can lead to persistent skin changes if ignored. By understanding toasted skin syndrome causes, monitoring symptoms, and implementing prevention strategies, you can protect your skin effectively.
Early recognition and proper management are key. Avoid prolonged heat exposure, monitor your skin, and consult a dermatologist if changes persist. Your skin health is worth the attention.