Abscess ICD 10 Code (2026): Types, Symptoms, Diagnosis, Treatment & Coding Guide
Guide to Types, Symptoms, Diagnosis & Treatment
Last Updated: January 2026
Table of Contents – Abscess ICD 10 Code Guide
What is an Abscess?
Abscess Types and Classifications
Importance of Abscess ICD-10 Coding
Common Abscess ICD-10 Codes
Causes of Abscesses
Symptoms of Abscesses
Diagnosis of Abscess
Treatment of Abscesses (Abscess ICD 10 Treatment Guidelines)
Prevention of Abscesses (How to Avoid Abscess ICD 10 Conditions)
Frequently Asked Questions (FAQs about Abscess ICD 10 Code)
Conclusion
Introduction
es are common localized infections that develop when the body responds to bacteria, fungi, or other pathogens. Proper identification and medical documentation are essential for accurate diagnosis, effective treatment, and long-term patient care. ICD-10 coding helps healthcare professionals classify abscesses based on their location, depth, and severity, ensuring consistency across clinical records, treatment plans, and insurance documentation.
What is an Abscess?
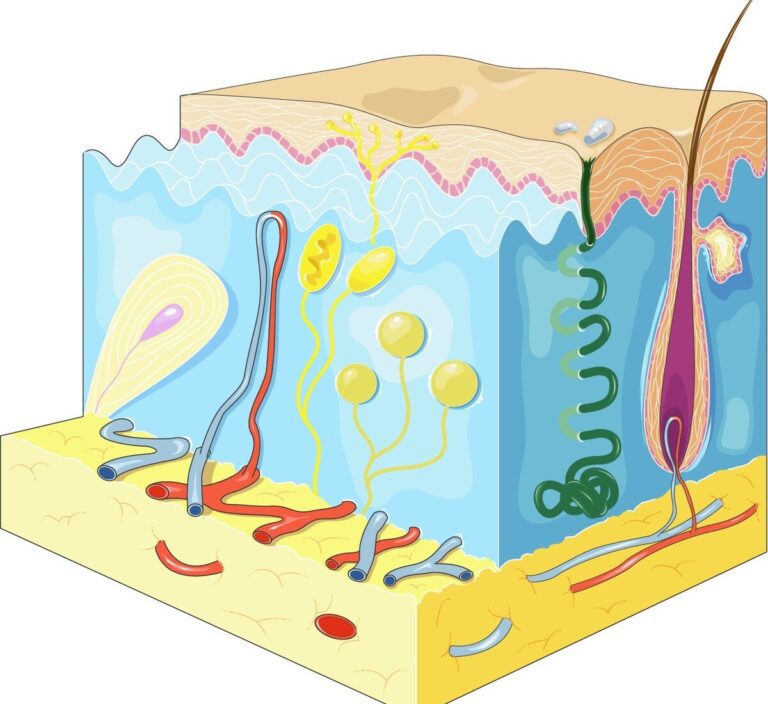
An abscess is a localized collection of pus that forms when the body’s immune system responds to infection. These infections are usually caused by bacteria, but sometimes fungi or viruses can trigger abscess formation. The immune system sends white blood cells to the affected area to fight the pathogens, resulting in a pocket of pus surrounded by inflamed tissue.
Abscesses can occur in any part of the body, from superficial layers like the skin to deeper tissues and organs such as the liver, lungs, brain, or kidneys. Superficial abscesses often appear as painful, red, and swollen lumps, while deep abscesses may remain hidden and cause systemic symptoms like fever, fatigue, or general malaise.
Untreated abscesses can lead to serious complications including:
- An infection of the surrounding skin and soft tissues is called cellulitis.
- Sepsis, or the spread of an infection into the bloodstream
- Irreversible tissue damage or scarring
The use of abscess ICD 10 code ensures accurate documentation of the abscess type, location, and severity. For instance, a back abscess is coded as L02.414, while an abscess of the right index finger is L02.531. Correct coding helps healthcare providers plan targeted treatment, facilitates insurance claims, and allows for epidemiological tracking of infection patterns.
Key Points:
- Abscesses are the body’s defensive mechanism against infection.
- Can be superficial (skin) or deep (internal organs).
- Proper coding using abscess ICD 10 code is essential for clinical management, billing, and public health tracking.
Abscess Types and Classifications
Abscesses can be classified based on location, depth, and underlying cause. Understanding the type of abscess is essential for accurate diagnosis, proper treatment, and correct documentation using abscess ICD 10 code. Here’s a detailed look at each type:
1. Cutaneous or Skin Abscesses

These are the most common type of abscess, appearing as red, swollen, and painful lumps on the skin, often referred to as boils or furuncles. They usually develop around hair follicles or minor skin injuries.
ICD-10 Examples:
- L02.9 – Other skin abscess
- L02.414 – Abscess of back
Key Points:
- Surface-level and easily noticeable
- Can often be managed with warm compresses or minor medical drainage
- Early detection prevents infection from spreading to deeper tissues
2. Subcutaneous and Soft Tissue Abscesses
These abscesses develop beneath the skin in connective tissue or muscles. They are less visible than cutaneous abscesses and may require ultrasound or other imaging for accurate detection.
Symptoms: Deep-seated pain, swelling without obvious skin changes, sometimes accompanied by fever or fatigue.
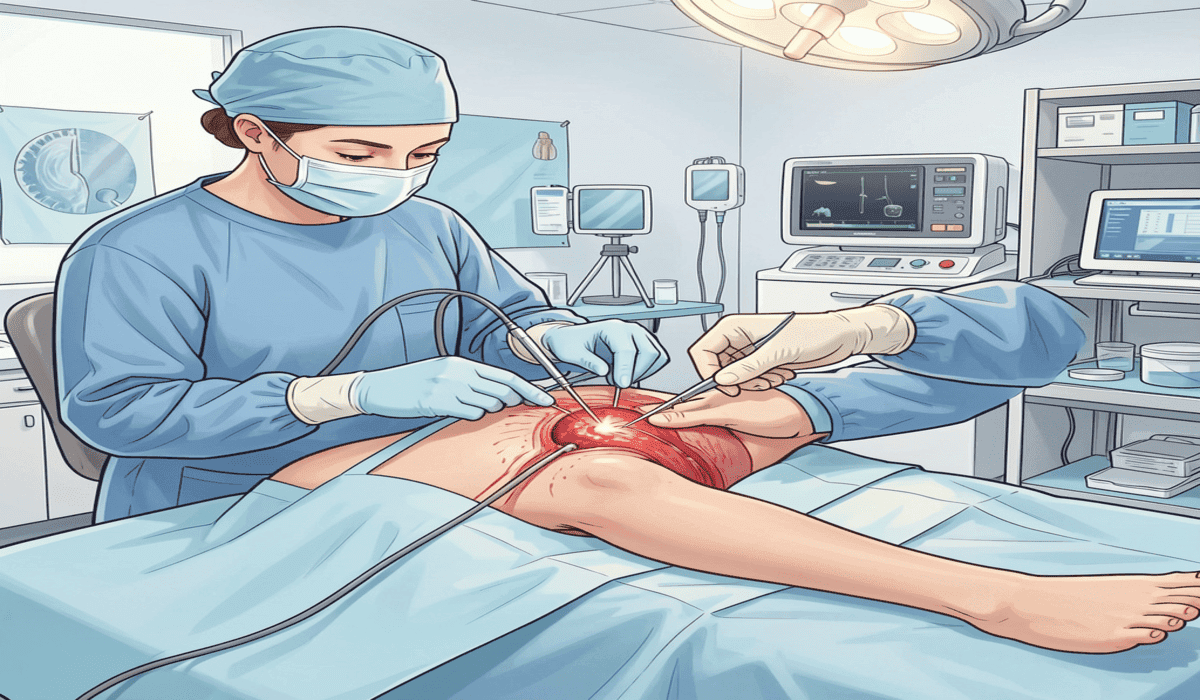
Treatment: Frequently calls for medical professionals to perform incision and drainage (I&D), occasionally in conjunction with antibiotics.
3. Internal Organ Abscesses
Abscesses can also form in internal organs such as the liver, brain, lungs, or kidneys. These are serious infections that usually do not present with visible signs until systemic symptoms occur.
Symptoms: Fever, chills, fatigue, nausea, abdominal pain (liver/kidney), or neurological symptoms (brain).
ICD-10 Examples:
- G06.0–Abscess of the brain
- K75.0 – Abscess of the liver
Diagnosis: Requires CT scans or MRI to detect and assess the extent of infection. These abscesses require urgent medical intervention to prevent life-threatening complications like sepsis.
4. Dental Abscesses
Dental abscesses occur in the teeth or gums, often due to untreated cavities or bacterial infections. These abscesses can cause intense localized pain, swelling, and sometimes fever.
ICD-10 Code: K04.7 – Periapical abscess with sinus
Treatment: Often involves drainage by a dentist, root canal, or tooth extraction, combined with antibiotics if infection has spread.
5. Perianal and Pelvic Abscesses
These abscesses develop in the rectal or pelvic region, causing pain during bowel movements or urination.
ICD-10 Example: K61.0 – Perianal abscess
Symptoms: Pain, swelling, redness near the anus, sometimes fever in severe cases.
Treatment: Typically requires surgical drainage, followed by antibiotics and hygiene management to prevent recurrence.
Pro Tip:
While superficial skin abscesses are common and often manageable at home, internal abscesses are much more dangerous. They require urgent medical attention, proper imaging, and correct classification using Abscess ICD 10 Code to ensure timely and effective treatment.
Importance of Abscess ICD 10 Coding
Accurate abscess ICD 10 code is a critical component of modern healthcare. It allows clinicians, coders, and insurance providers to categorize abscesses correctly, ensuring that patients receive proper care and medical records remain precise.
Here’s why using the correct abscess ICD 10 code matters:
1. Accurate Medical Records
Correct coding ensures that a patient’s medical history reflects the exact type, location, and severity of the abscess. This allows healthcare professionals to monitor treatment progress, track recurrence, and make informed decisions about follow-up care.
2. Insurance Claims and Billing Compliance
Using the proper ICD 10 code is essential for insurance processing and reimbursement. Incorrect coding can lead to claim denials, delays in treatment approval, or financial discrepancies. Accurate documentation guarantees that patients and healthcare facilities are protected from billing issues.
3. Tracking Infection Patterns
By coding abscesses consistently, hospitals and public health agencies can monitor trends, identify outbreaks, and study infection patterns. This is especially important for bacterial infections like Staphylococcus aureus, which are a common cause of abscesses.
4. Streamlined Clinical Communication
Correct ICD-10 coding facilitates clear communication between clinicians, coders, and specialists. When every healthcare provider understands the exact type and location of an abscess, treatment planning becomes more efficient and precise.
5. Preventing Legal or Diagnostic Errors
Using the wrong ICD-10 code can lead to misdiagnosis, inappropriate treatment, or even legal complications. Accurate coding ensures that all medical, insurance, and legal documentation reflects the patient’s true condition.
Pro Tip:
Always double-check the abscess ICD 10 code based on location, severity, and type. For example, a back abscess is coded as L02.414, while a perianal abscess uses K61.0. Using the correct code avoids claim denial, ensures proper care, and improves patient outcomes.
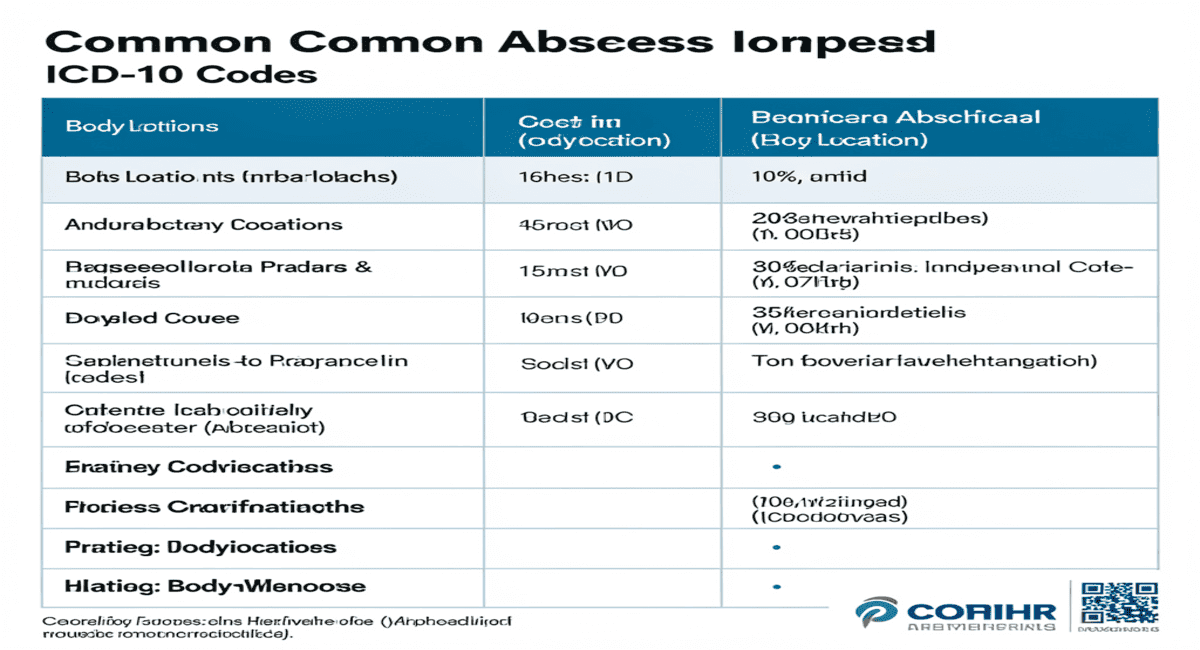
Common Abscess ICD 10 Code
Accurate abscess ICD 10 code are essential for proper medical documentation, insurance claims, and treatment planning. The table below lists the most commonly used codes, organized by abscess location and type:
| Location | ICD 10 Code | Description |
| Back | L02.414 | Cutaneous abscess of back |
| Face | L02.21 | Abscess of face |
| Groin | L02.91 | Abscess of groin |
| Right Index Finger | L02.531 | Finger abscess |
| Other Skin Abscess | L02.9 | Unspecified skin abscess |
| Perianal | K61.0 | Anorectal abscess |
| Dental | K04.7 | Periapical abscess |
| Brain | G06.0 | Intracranial abscess |
| Liver | K75.0 | Liver abscess |
Key Notes for Using Abscess ICD 10 Code
- Location Matters: Always assign the code based on the exact anatomical site of the abscess. For example, an abscess on the back differs from one on the groin.
- Severity Consideration: Some ICD-10 codes may vary depending on depth or complications; internal organ abscesses require accurate imaging-based diagnosis.
- Avoid Errors: Misclassification can lead to insurance claim denials, miscommunication, and treatment delays.
- Documentation: Pair the code with detailed notes on size, pus presence, and systemic symptoms for complete medical records.
Pro Tip:
Using Abscess ICD-10 Codes accurately helps clinicians track infection patterns, monitor treatment outcomes, and ensures efficient healthcare delivery. Always double-check the code for each abscess type and location.
Causes of Abscesses
Understanding the causes of abscesses is essential for prevention, accurate diagnosis, and proper documentation using abscess ICD 10 code. Abscesses occur when the body reacts to infections or injuries, leading to a localized collection of pus. Multiple factors contribute to abscess formation:
1. Bacterial Infections
The most common cause of abscesses is bacterial infection, particularly Staphylococcus aureus and Streptococcus species. These bacteria can enter the body through:
- Small wounds or scrapes
- Puncture-related injuries
- Hair roots
Once inside, the immune system sends white blood cells to fight the infection, causing pus accumulation and swelling.
Correct abscess ICD 10 code helps track bacterial infection patterns, guide treatment, and monitor recurrence.
For similar skin infections, see Fungal Acne Treatment at Home or Clogged Pores on Breasts: Tips & Remedies.
2. Blocked Sweat or Oil Glands
Obstructed sweat or sebaceous (oil) glands create a favorable environment for bacteria, leading to boils or hidradenitis suppurativa. These abscesses often appear in areas like the armpits, groin, or back.
Tip: Regular hygiene, exfoliation, and avoiding tight clothing can reduce risk. Accurate coding using abscess ICD 10 code ensures proper clinical documentation for recurrent cases.
3. Minor Trauma or Ingrown Hairs
Even small injuries such as scratches, insect bites, or ingrown hairs can allow bacteria to penetrate deeper layers of skin, causing an abscess.
- Redness, tenderness, and swelling may appear within days
- Early detection prevents progression to larger abscesses
ICD 10 Coding: Superficial abscesses like L02.9 (Other skin abscess) or localized abscesses such as L02.531 (Finger abscess) should be documented for treatment and follow-up.
4. Weakened Immune System
Individuals with a compromised immune system—due to HIV, chemotherapy, or prolonged steroid use—are at higher risk of abscess formation.
- The body is unable to successfully combat infections.
- Multiple or severe abscesses may form
Accurate abscess ICD 10 code are essential in these cases to track infection severity and plan specialized care.
5. Underlying Medical Conditions
Chronic health conditions like diabetes, obesity, or vascular disease increase susceptibility to abscesses.
- High blood sugar in diabetes can impair healing
- Obesity and poor circulation increase infection risk
Documenting abscesses with the correct ICD-10 code ensures clinicians provide targeted treatment while maintaining comprehensive medical records.
Pro Tip:
Preventing the above causes—through proper hygiene, wound care, and management of chronic conditions—significantly reduces the incidence of ICD-10-coded abscesses. Early intervention and accurate coding help streamline treatment, insurance claims, and follow-up care.
Symptoms of Abscesses
Recognizing the symptoms of an abscess early is critical for effective treatment, prevention of complications, and accurate documentation using Abscess ICD-10 Codes. Symptoms can vary depending on location, depth, and severity of the infection, but certain signs are common across most abscess types.
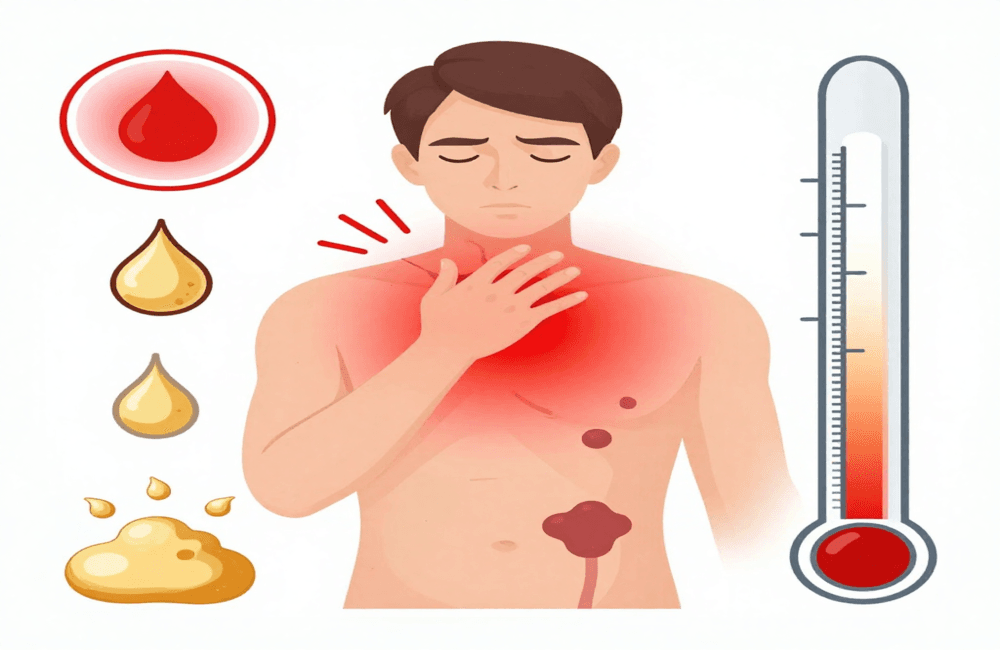
1. Redness, Swelling, and Warmth
One of the first noticeable signs of an abscess is localized redness, swelling, and warmth at the infection site. This occurs due to increased blood flow as the immune system sends white blood cells to combat infection.
- Superficial skin abscesses like boils or furuncles are often visible and tender
- Internal abscesses may cause swelling and discomfort in deeper tissues
ICD-10 Tip: Accurate documentation with codes such as L02.414 (back abscess) or K61.0 (perianal abscess) helps clinicians track infection location and severity.
2. Localized Pain and Tenderness
Pain is a hallmark of abscess formation. The intensity can vary:
- Mild tenderness for small superficial abscesses
- Severe, throbbing pain in deep or larger abscesses
Pain increases when pressure is applied or the abscess grows. Correctly identifying the site helps assign the right Abscess ICD-10 Code for targeted treatment.
Clogged Pores on Breasts and Itchy Rash on Neck: Causes & Treatment are related painful skin ailments.
3. Pus Discharge
As the abscess progresses, it may rupture, releasing thick yellow or green pus, often foul-smelling.
- This indicates the immune system is actively fighting infection
- Drainage is sometimes performed medically to prevent further spread
Proper documentation using Abscess ICD-10 Codes ensures follow-up care and tracks the site of infection.
4. Fever, Chills, and Fatigue
Severe abscesses, especially internal organ abscesses, can produce systemic symptoms:
- Fever and chills indicate the infection may have entered the bloodstream
- Fatigue and malaise are common in widespread infection
ICD-10 Tip: Internal abscesses like G06.0 (brain) or K75.0 (liver) require careful coding to monitor treatment and complications.
5. Swollen Lymph Nodes
Lymph nodes near the affected area may enlarge as the body fights the infection. This is especially common in:
- Facial abscesses
- Painful infections near the groin region
Monitoring lymph node swelling supports diagnosis, treatment planning, and ICD-10 documentation.
6. Restricted Movement (if near muscles or joints)
Abscesses located in or near muscles or joints may restrict movement due to pain and inflammation. Early recognition prevents tissue damage or chronic complications.
Pro Tip: Document all symptoms carefully with the appropriate Abscess ICD-10 Code to ensure accurate patient records and guide clinical decisions.
Summary:
Early recognition of redness, swelling, pain, pus discharge, fever, lymph node swelling, and restricted movement allows for timely intervention.
Correct Abscess ICD-10 coding ensures proper treatment, insurance processing, and follow-up care, preventing complications like cellulitis, sepsis, or chronic abscess formation.
Diagnosis of Abscess
Accurate diagnosis of an abscess is critical for proper treatment, preventing complications, and ensuring correct documentation using abscess ICD 10 code. Because abscesses can vary in size, depth, and location, healthcare providers use a combination of clinical evaluation, imaging, and laboratory tests to confirm the diagnosis.

1. Physical Examination
The first step in diagnosing an abscess is a thorough physical exam:
- The clinician looks for redness, warmth, swelling, and tenderness
- A fluctuant or soft mass under the skin often indicates pus accumulation
- Determining the exact location is essential for accurate Abscess ICD 10 coding (e.g., L02.414 for back abscess or L02.91 for groin abscess)
2. Medical History Review
A detailed medical history provides crucial context:
- Previous skin infections or abscesses
- Chronic conditions like diabetes, obesity, or immune disorders
- Recent trauma, cuts, or insect bites
- Current medications, especially steroids or immunosuppressants
Understanding the patient’s history helps distinguish simple abscesses from recurrent or deep infections and ensures correct ICD-10 documentation.
Learn more about immunity concerns in Shower Hair Loss: Causes & Remedies, and understand common skin infections through our Clogged Pores on Breasts guide.
3. Imaging Tests
For deep or internal abscesses, imaging is often required:
- Ultrasound: Confirms fluid-filled cavities in soft tissue
- CT Scan / MRI: Essential for abscesses in organs like liver, brain, lungs, or pelvis
Imaging results guide surgical drainage or medical therapy and help assign the correct abscess ICD 10 code for documentation and insurance claims.
4. Laboratory Tests and Bacterial Cultures
To identify the causative pathogen:
- Pus is collected and sent for bacterial culture and sensitivity testing
- Streptococcus species and Staphylococcus aureus are common pathogens.
- Results help select effective antibiotics and prevent recurrence
Accurate lab results paired with abscess ICD 10 code ensure proper tracking of infection patterns and patient follow-up.
5. Differential Diagnosis
Not all lumps or swellings are abscesses. Physicians may need to rule out:
- Cysts: Non-infectious fluid-filled sacs
- Tumors: May mimic abscess symptoms
- Cellulitis: Skin infection that can occur with or without abscess formation
Differentiating ensures precise ICD 10 classification and prevents treatment errors or legal complication
Summary:
The diagnosis of an abscess involves: physical exam, medical history, imaging, lab tests, and differential diagnosis. Correct evaluation allows healthcare providers to assign the accurate abscess ICD 10 code, plan effective treatment, and maintain standardized, reliable medical records.
Treatment of Abscesses (Abscess ICD 10 Treatment Guidelines)
Proper treatment of an abscess is essential to relieve pain, prevent infection spread, and ensure complete healing. Treatment strategies depend on the size, depth, location, and severity of the abscess. Following abscess ICD 10 code helps clinicians document care accurately and track outcomes for insurance and follow-up purposes.
Home Care for Small or Superficial Abscesses
For minor abscesses close to the skin surface, home management can often be effective. However, early care is essential to prevent progression:
- Warm Compress
- Use three to four times daily, letting it sit for 10–15 minutes each time.
- Helps increase blood circulation, encouraging natural drainage
- Maintain Cleanliness
- Clean the affected spot carefully using a gentle antibacterial soap
- Steer clear of rough scrubbing as it can cause skin irritation.
- Refrain from Puncturing or Squeezing
- Attempting to pop an abscess can push bacteria deeper, causing serious infection or sepsis
- Topical Treatments
- Over-the-counter antiseptic creams or antibiotic ointments can reduce bacterial growth
- Example: Neosporin or other clinically approved topical antibiotics
Explore home remedies in Fungal Acne Treatment at Home, and discover more skincare guidance in Itchy Rash Under Breast: Causes & Prevention
Medical Treatments for Abscesses
For large, deep, or high-risk abscesses, professional medical care is required. Accurate documentation using abscess ICD 10 code ensures proper treatment planning, insurance processing, and follow-up care.
- I&D procedure for abscesses
- The most common and effective procedure for draining large abscesses
- Reduces pain, pressure, and risk of infection spread
- Done under strict aseptic conditions
- Antibiotic Therapy
- Prescribed if the abscess is deep, multiple, or systemic
- Common antibiotics include Clindamycin, Cephalexin, or Doxycycline
- The choice of the most suitable antibiotic is guided by the results of culture and sensitivity testing.
- Pain Management
- Over-the-counter painkillers like Ibuprofen or Acetaminophen help control pain and reduce inflammation
- Pain management is essential for maintaining mobility and comfort
- Follow-Up Care
- Regular dressing changes and wound cleaning
- Monitoring for recurrence, swelling, or new symptoms
- Patients with diabetes, immune compromise, or chronic conditions require closer supervision
For expert advice on wound care, see CDC Guidelines for Skin Infections.
Special Considerations
- Patients with Diabetes: Healing may be slower, and infections can worsen rapidly
- Immune-Compromised Individuals: Higher risk of recurrent or systemic abscesses
- Internal Abscesses: Abscesses in organs (liver, brain, lungs) require surgical intervention, hospitalization, and precise ICD-10 coding
Summary:
Effective abscess treatment combines home care for minor cases and medical intervention for severe cases. Following abscess ICD 10 code ensures proper documentation, guides treatment, and supports follow-up care. Early and correct management prevents complications like cellulitis, sepsis, or chronic abscess formation.
Prevention of Abscesses (How to Avoid Abscess ICD 10 Conditions)
Preventing abscesses is far easier than treating them, especially since bacterial infections, particularly Staphylococcus aureus, are the most common cause. Adopting simple hygiene practices, timely wound care, and healthy lifestyle habits can significantly reduce the risk of developing abscesses, which are tracked and categorized using abscess ICD 10 code.
1. Maintain Proper Hygiene
- Daily Cleaning: Wash your body daily with gentle, antibacterial soap to remove dirt, sweat, and bacteria that can clog pores.
- Moisturize Skin: Keep skin hydrated to prevent cracks or dryness that may allow bacteria to enter.
- Avoid Harsh Products: Use mild, pH-balanced cleansers to maintain the natural skin barrier.
For related skin care tips, see Best Sunscreen for Oily Skin: Top Picks and Cetaphil Gentle Skin Cleanser Review 2025.
2. Treat Minor Wounds Immediately
Even tiny wounds can become potential entry points for harmful bacteria. Quick care reduces the risk of abscess formation.
- Clean Wounds: Rinse with clean water and mild soap.
- Apply Antiseptic: Use clinically approved antiseptic cream or solution.
- Cover Wounds: Use sterile bandages until fully healed.
Pro Tip: Timely wound care also supports accurate documentation under abscess ICD 10 code, especially for insurance purposes.
3. Avoid Sharing Personal Items
Sharing items like razors, towels, or clothing can transfer bacteria and increase abscess risk.
- Use your own towels and grooming tools.
- Disinfect frequently used items with antiseptic solutions.
Related precautions can be found in Fungal Acne Treatment at Home: 15 Proven Remedies.
4. Manage Chronic Conditions
Underlying health conditions like diabetes, obesity, or immune disorders can increase susceptibility to abscesses.
- Monitor Blood Sugar: For diabetic patients, controlled blood sugar reduces infection risk.
- Support your body’s defenses with a balanced diet, proper hydration, and adequate sleep.
- Regular Medical Checkups: Early detection of infections prevents complications requiring ICD 10 coded interventions.
See Health Tips for Women: How to Stay Fit and Healthy for lifestyle and immunity-boosting tips.
5. Wear Clean and Breathable Clothing
- Choose Breathable Fabrics: Cotton or moisture-wicking fabrics reduce sweat buildup.
- Avoid Tight Clothing: Prevents friction and bacterial growth, especially in high-risk areas like groin, back, and underarms.
Pro Tip: Proper clothing and hygiene practices are simple but effective ways to prevent abscesses classified under Abscess ICD-10 Codes.
Summary:
Preventing abscesses involves maintaining hygiene, treating wounds promptly, avoiding shared personal items, managing chronic conditions, and wearing clean clothing. These practices not only lower infection risk but also reduce the need for complex treatments documented under abscess ICD 10 code.
Frequently Asked Questions (FAQs about Abscess ICD 10 Code)
Here are the most common questions about abscesses and their documentation using abscess ICD 10 code, along with expert answers to guide patients and healthcare providers.
Q1. What is the ICD 10 code for a back abscess?
The ICD-10 code for a cutaneous abscess of the back is L02.414.
- This code is used by healthcare providers and coders to document the condition accurately for medical records, insurance claims, and treatment tracking.
- Accurate coding helps ensure proper follow-up care and epidemiological tracking.
See Common Abscess ICD 10 Codes (2026 Updated Table) for codes of other body parts.
Q2. Can abscesses heal without treatment?
- Small or superficial abscesses may sometimes resolve on their own with proper hygiene, warm compresses, and topical care.
- Most abscesses require a combination of I&D and antibiotics to control and prevent the spread of infection.
- Untreated abscesses can lead to cellulitis, systemic infection, or sepsis, making early medical care essential.
Internal Link Suggestion: For at-home management, see Treatment Guidelines for Abscess.
Q3. Are abscesses contagious?
- Most abscesses are not highly contagious.
- Bacteria within the pus (like Staphylococcus aureus) can spread if pus comes into contact with broken skin of another person.
- Proper hygiene, wound care, and avoiding shared personal items reduce transmission risk.
Internal Link Suggestion: See Prevention of Abscesses for detailed safety tips.
Q4. Why is abscess ICD 10 code important?
- Correct abscess ICD 10 code are crucial for:
o Proper documentation of the condition in medical records
o Insurance claims and billing compliance
o Effective clinical communication between doctors, nurses, and coders
o Guiding treatment planning based on abscess location, type, and severity
- Inaccurate coding can lead to claim denial, treatment errors, or legal issues.
Q5. How can recurrent abscesses be prevented?
- Follow strict personal hygiene practices to reduce bacterial exposure.
- Manage chronic conditions like diabetes or immune disorders to strengthen the body’s infection-fighting ability.
- Promptly treat cuts, scrapes, or minor infections to prevent progression into abscesses.
- Wear clean, breathable clothing and avoid sharing personal items to minimize bacterial transmission.
Internal Link Suggestion: See Prevention of Abscesses for a complete guide.
Conclusion
Abscess ICD 10 codes are essential for accurately documenting, diagnosing, and treating abscesses. Using the correct abscess ICD 10 code ensures early recognition, helps prevent serious complications such as sepsis and cellulitis, and guides timely medical care, including effective drainage and antibiotic therapy. Proper coding also streamlines insurance claims, supports clear clinical communication, and aids in tracking patient outcomes. Additionally, maintaining hygiene and managing chronic conditions further reduces the risk of recurrent abscesses.
Disclaimer
This text is solely intended for educational and informational purposes. It does not replace professional medical advice, diagnosis, treatment, or official ICD-10 coding guidance. Always consult a qualified healthcare provider or certified medical coder for accurate medical care and coding.